The recognition of ST-segment elevation myocardial infarction (STEMI) in the presence of left bundle-branch block (LBBB) remains difficult and frustrating to both emergency medicine physicians and cardiologists. According to the 2004 STEMI guidelines, emergent reperfusion therapy was recommended to patients with suspected ischemia and new LBBB however, the new 2013 STEMI guidelines made a drastic change by removing this recommendation. Several papers have recently been published discussing a modified Sgarbossa’s criteria and a new algorithm to help decrease false cath lab activation and/or fibrinolytic therapy, but are they ready for primetime?
The recognition of ST-segment elevation myocardial infarction (STEMI) in the presence of left bundle-branch block (LBBB) remains difficult and frustrating to both emergency medicine physicians and cardiologists. According to the 2004 STEMI guidelines, emergent reperfusion therapy was recommended to patients with suspected ischemia and new LBBB however, the new 2013 STEMI guidelines made a drastic change by removing this recommendation. Several papers have recently been published discussing a modified Sgarbossa’s criteria and a new algorithm to help decrease false cath lab activation and/or fibrinolytic therapy, but are they ready for primetime?
What were the old guidelines for LBBB and STEMI activation?
- 1996 and 2004 American College of Cardiology/American Heart Association (ACC/AHA): Class I indication if symptoms < 12 hours1,2
- 2012 European Society of Cardiology (ESC): Class Ia indication if symptoms < 12 hours3
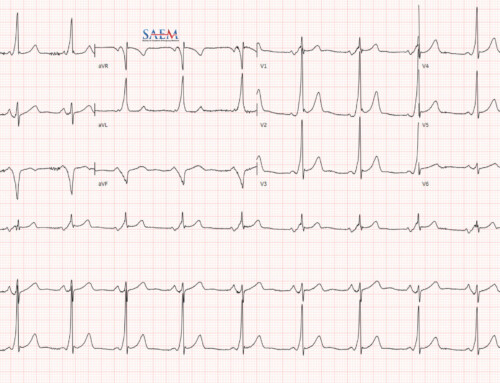
Original Sgarbossa Criteria
- Concordant ST-segment elevation ≥ 1 mm in any lead (5 points)
- Concordant ST-segment depression ≥ 1 mm in lead V1 – V3 (3 points)
- Discordant ST-segment elevation ≥ 5 mm in any lead (2 points)
How accurate are the old Sgarbossa Criteria?
In detecting culprit coronary occlusion on angiography, the rate of false activation with STEMI and presumed new LBB was:
- Larson et al: 44%5
- Chang et al: 80.8%6
- Jain et al: 86%7
Ideally, diagnostic tests for life-threatening conditions (i.e. AMI) need to be highly sensitive. The reason the original Sgarbossa criteria are limited in clinical practice is the low sensitivity (20%). This is why a new LBBB alone is no longer a criteria for emergent cath lab activation. Recently, Steven Smith, MD from Dr. Smith’s ECG Blog published a new criterion to replace the third component of the original Sgarbossa Criteria using the ST/S ratio instead of discordant ST-elevation ≥ 5mm.
What are the new modified Sgarbossa Criteria?
- Concordant ST-segment elevation ≥ 1 mm in any lead
- Concordant ST-segment depression ≥ 1 mm in lead V1 – V3
- Discordant ST/S Ratio ≤ -0.25
How should the modified Sgarbossa Criteria be used in initial evaluation of patients with suspected AMI with LBBB?4
- Suspected patient with AMI with LBBB should have emergent primary PCI or fibrinolysis if:
- Hemodynamic instability or acute heart failure (Validated), or
- Sgarbossa score ≥ 3 (Validated), or
- ST/S ratio ≤ -0.25 (Proposed, NOT Validated)
Limitations of the modified Sgarbossa Criteria and the proposed new algorithm
- The ST/S ratio study is a very small study (33 vs 129 ECGs)
- More complex, making the modified criteria and algorithm harder to remember
- Need a prospective, externally validated study to confirm clinical application of the modified Sgarbossa Criteria
Take Home Point
The Modified Sgarbossa Criteria is more sensitive than the original Sgarbossa Criteria for predicting AMI in the presence of LBBB, but needs an external validation study before we can begin to apply it.