|
|
|
|
|
|
A newsletter for medical students pursuing a career in emergency medicine
|
|
|
|
|
Letter from the Editor:
Hello #EMBound Med students,
|
It is the 2 year anniversary of the ALiEM EM Bound newsletter! In reflecting over this time, we have weathered many things together: a global pandemic, the often uncertain path to EM, ERAS and interview considerations, and of course the Match. We have shared wellness tips, amazing resources like EM Over Easy, and ways to shine on your rotation through our rotation round-up.
|
We are thankful to be part of your journey, and hope to grow as we learn your needs. Please fill out our Feedback Form to help us serve you better! We look forward to continuing this path to helping you become #EMBound and welcoming you into our specialty as colleagues & friends.
|
|
--Sree Natesan, MD Editor-in-Chief
|
|
|
|
|
|
CLERKSHIP LIFE &
RESIDENCY APPLICATION SEASON
|
Reflections on Emergency Medicine
David Gordon, MD
|
Undergraduate Educations Director
|
As one application season has concluded with the completion of The Match and another season begins with away rotations, I wanted to reflect on the question “why choose Emergency Medicine (EM)?” Some of you may be firmly committed to EM as a career choice whereas for others EM is one of several specialties being considered. The reasons to choose EM which I share below are not just my own, but also those expressed by the talented applicants I got to meet this year. While the reasons are numerous, I have grouped them into three main themes:
|
- Intellectual: Emergency Medicine offers the excitement of the unexpected and unknown. Each shift is unique with a variety of patient presentations that span different medical specialties and diverse patient demographics. In the ED, emergency physicians are the first ones to lay eyes and hands on undifferentiated patients and have to think both critically and creatively about their diagnosis and treatment. In critical care situations, emergency physicians must quiet the mind to act methodically and decisively in life and death scenarios. EM offers great reward for those who enjoy being intellectually challenged as we must utilize the arsenal of medicine to figure out the best way to serve every patient that enters the ED.
- Relational: When it comes to interprofessional relationships, emergency medicine functions as a team sport. It is a specialty with a horizontal hierarchy reflected in close working relationships among attendings, residents, and students. Emergency physicians enjoy and depend on their collaboration with other health professionals including nursing, mid-level providers, paramedics, social workers, respiratory therapists, and more. With respect to patient care, emergency physicians are privileged with supporting patients and their families through moments of fear, hardship, and sometimes loss. The immediacy and significance of these moments bring great value and meaning to one’s career.
- Spiritual: Medicine is a profession rooted in service to humanity. No where is that mission more strongly manifested than in Emergency Medicine, and each year I see this increasingly recognized by and resonating with EM applicants. No matter the issue, the time of day, or one’s ability to pay, the doors of the ED are always open. There is a dignity and nobility in the role that ED’s play in the healthcare system which provides a big draw to EM and a reason one can feel good after every shift. The global pandemic recognized this during their #healthcareheros campaign. In that national shut-down, it was our field that showed up to do what we have done long before the pandemic, and will continue to do long after: to serve our community.
No matter where you are on the spectrum: whether you have no idea what specialty you want to do or you are about to embark on your training in an EM residency, it can be helpful to reflect and connect with what brings you enjoyment and sense of purpose. Not every day may be your best, but when your profession aligns with your core values, you know you have made the right choice.
|
|
|
|

|
|
|
We know there is so much more to medicine than what the classroom and even rotations provide. Truly practicing good medicine involves critical conversations, understanding social dynamics, and a few good laughs too. In EM over Easy, we talk about topics from resiliency and productivity to social topics about gender, depression, and physician suicide. We also cover clinical topics with a more than medicine twist and inject humor into the mix.
|
|
To be a part #MoreThanMedicine conversation, listen to the EM Over Easy Podcast with EM docs and hosts Andy Little, Tanner Gronowski, Drew Kalnow, and John Casey.
|
Find us at www.emovereasy.com, @emovereasy on Twitter, and on your favorite podcast player!
|
|
|

|
ROTATION TUNE-UP
Arm yourself with Clinical Tools
|
|
In this series, we will be looking into commonly available tips and tricks, guidelines, algorithms, and clinical decision-making scores relevant to your clerkship rotation. Our goal is to augment your presentations on shift and set you up for success. We hope that you find this new series helpful as you embark on your journey to emergency medicine.
|
|
|
|
Headaches
Sree Natesan, MD
|
Associate Program Director
|
Duke University Emergency Medicine
|
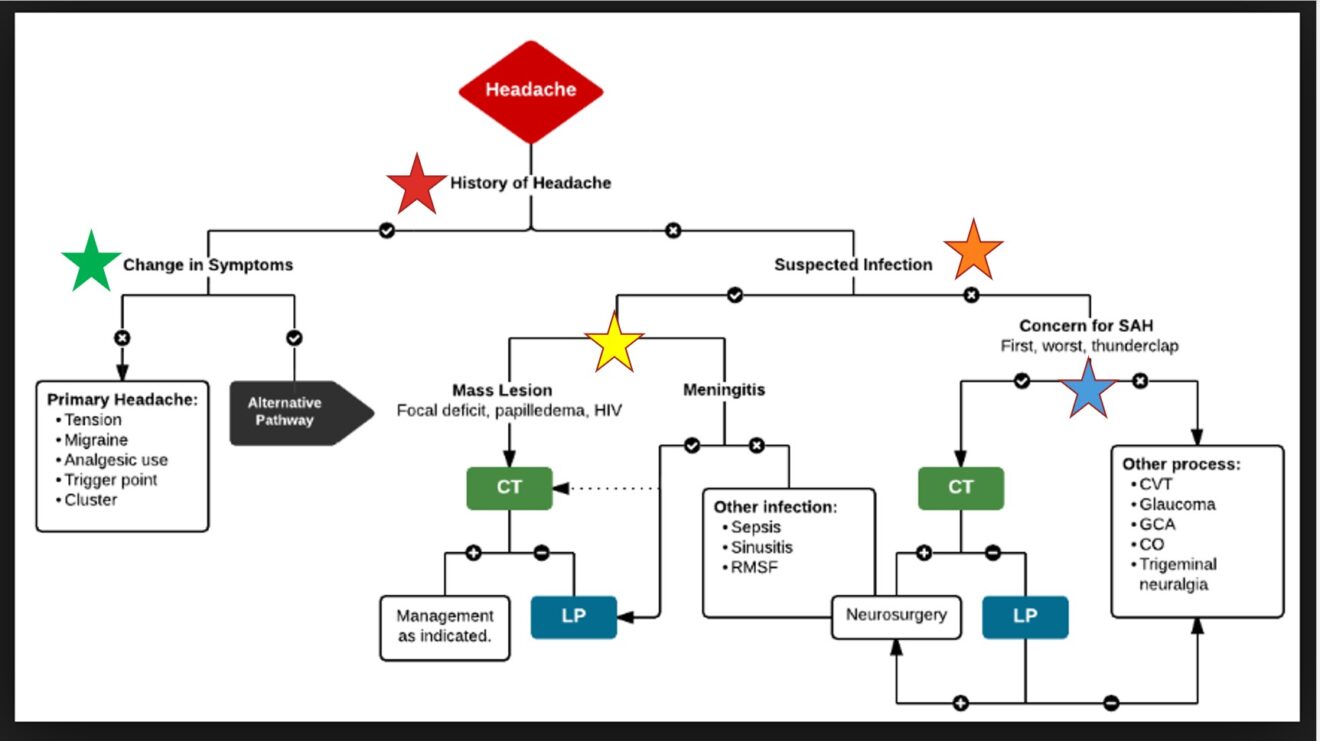
Headaches (H/A) are a common presentation to the Emergency Department. You may feel your own head ache as you try to figure out what the differential diagnosis and plan should be for the patient you are caring for in the ED. Having a systematic approach to these patients can help you in your efficiency and accuracy in obtaining the right clues to lead you to the diagnosis. Here are some pearls:
|
- History: A thorough history can help you elicit the etiology of the H/A. Here are a few considerations:
- Onset: The onset of the H/A can really be the best place to start. Sudden onset, "thunderclap" can suggest a vascular etiology. A more gradual course may suggest an infectious or inflammatory etiology, whereas a progressive headache or neuro symptoms may suggest a malignancy etiology.
- Character: While a lot of patients will say they are having the "worst headache of their life," not all of them are having a subarachnoid hemorrhage (SAH). Asking questions such as "what number was the pain when it started, what is the pain level now," or "did it come on gradually versus all of a sudden" can help you learn more. Another question is asking "when did you have a headache this bad" can gather the idea if this is the worst headache or not. A careful history is important.
- Associated symptoms: Its key to do a good ROS. If the patient is having fever and neck stiffness, then meningitis would jump up on the DDx. If the patient is having an aura and photophobia, then migraine may be the culprit.
- Physical exam: Your exam is key to helping to elucidate the working DDx and guide your workup. Here are a few pearls to make sure you focus on when your patient presents with H/A:
- Eye Exam: A fundoscopic exam looking for papilledema can help you figure out if your patient has increased intracranial pressure (ICP) in processes such as Idiopathic Intracranial Hypertension (Pseudotumor Cerebri) or space occupying lesions like meningiomas, glioblastomas, metastatic disease).
- Neuro Exam: You can localize the lesion (if one is present), based on your neurologic exam! It really is a map to the brain. Ensuring a thorough neuro exam means cranial nerves, strength, sensation, and reflexes. Cerebellar testing looking for nystagmus, abnormal finger-to-nose, heel-to-shin, or gait is important.
- Diagnostic/Therapeutics: The workup for H/A is really dependent on your thoughts on what the leading diagnosis is. For example, if you are worried about an infection, a lumbar puncture to analyze the fluid would be important. If your patient may have Pseuodotumor, an opening (and closing!) pressure from the spinal tap is key to the diagnosis. If you are worried about malignancy, imaging will be helpful (such as CT or MRI).
|
|
|
|
|
|
|
|

|
SPOTLIGHT
|
Anyone, Anything, Anytime… Anywhere:
Global Health in EM
Stanford Emergency Medicine
|
For many people, Medicine is a means to explore other professional interests as well. Emergency Medicine, some might argue more so than other specialties, is a skill set that is “mobile” and can be applied in a variety of leadership settings. Global Health or International Health is a cornerstone of Emergency Medicine and draws many residents to elective rotations and additional fellowship training.
|
- What is it?
- Global/International EM is more than mission-trips, humanitarian aid, and disaster response. Core to the mission of Global/International EM is sustainability through capacity building, collaborations with communities, and development of emergency response systems.
- Why is it important? Who does it benefit?
- Many countries still do not have EM as a medical specialty. The U.S. was the first country to recognize a dedicated field for emergency triage and management of the acutely ill or injured, undifferentiated patient. Most other parts of the world work with a structured healthcare system adopted the Franco-German model where subspecialists triaged to their respective inpatient units.
- Through the years, and as a result of various international natural and humanitarian disasters, EM emerged as a medical specialty that engages with direct provision of care. A few examples are through organizations such as Medecins Sans Frontieres (Doctors Without Borders), and the development of emergency management systems, such as through the World Association for Disaster and Emergency Medicine (WADEM).
- Through collaboration with other EM subspecialties, such as Ultrasound, Education, and Pediatrics, Global/International EM providers share knowledge and best practices with local healthcare providers to empower the care they provide to the communities they serve.
- How can I get involved?
- There are roughly 50 Global/International EM fellowships. Each program may define a specific focus for fellows and applicants may be attracted by the existing connections with other countries that are already in place.
- Often fellows will explore advanced education in either Tropical Medicine and Hygiene or a Masters of Public Health in Epidemiology.
- Given the added complexity of scholarship work across borders, it is important for those interested in Global/International EM to seek mentorship early and begin to form strong networks with the communities that they are interested in working with.
|
|
|

|
WELLNESS CORNER
|
Embrace the Discomfort of Change
Stanford Emergency Medicine
|
Spring signals change. For the Class of 2022, congratulations! The Match is over, and you can relax as you prepare for the intern year. For the Class of 2023, welcome!
|
In every transition, there comes this moment of this discomfort. It’s exciting and also scary. For the graduating seniors, this means figuring out what you’re going to do with the drop in adrenaline. Do you stay local? Do you travel? It’s probably too late to join an international rotation. Whatever you decide, here’s some advice. In 5 years or 10 years, what would you remember more from the last month of free time before being a full-time professional emergency medicine doctor?
|
For some of you, this means traveling and spending some time with the friends you made during medical school. For some, this may mean finishing up your research or capstone project. And for some, you’ll start opening up the books to prepare yourself for the internship year. Whatever you decide, pause. Enjoy the fact that you’ve finally arrived at a point in your life where you were so worried about where you would end up this time last year. Revel in this. You’ve earned it!
|
For those about to embark on the 2022-2023 application cycle, this means preparing for your away rotations, studying, planning your summer. Again, pause. You don’t have to figure it all out all at once. Reach out to some graduating medical students and ask them for tips. What did they learn? What were some lessons they took away from last year’s cycle? If they had to do it again, what would they do differently? What would they do again? They are your closest source of real-life experience from an applicant's perspective.
|
|
All the same, may you continue to find ways to enjoy your time as a medical student. May you go through transitions with ease and grace. It’s truly a privilege to be a part of a more significant force that helps our community through advancing science and alleviating suffering.
|
|
|
|

|
EXPAND YOUR
SOCIAL MEDIA HORIZONS
|
|
|
|
Now that Match Day is behind us, for program directors and #EMbound students alike, April begins the start of another application cycle. Welcome to the 2022-2023 recruitment season! Check out our past issues to get acquainted with our materials, and also welcome to those just joining us, and congratulations to those who are a few months away from graduation. Here's some great content in #SoMe:
|
|
|
|
|
|
|
|

|
EM MATCH ADVICE PODCAST
|
Welcome to the new academic year! The EM Match Advice series of podcasts are for senior EM medical students, co-hosted by Dr. Michael Gisondi and Dr. Michelle Lin. Check it out for some great tips to help you shine on your rotation.
|
|
|
|

|
ALiEM HIGHLIGHT REEL
|
|
The 3 most popular blog posts relevant for medical students in MARCH 2022 were the following:
|
|
|
|
|
|
|
|

|
EM Study Resources
|
|
|
|
Reminder: Bridge to EM is designed to help you through this 8-week guide to provide structured preparation that is free for students. It contains vetted up-to-date information to help you shine on your ED rotation. If you are looking to brush up on knowledge, or get a glimpse of what this specialty entails, check out this awesome resource!
|
|
|
|
|
|
|
We LOVE Feedback; We want to hear from you! Please take this short survey to help us continue to grow this resource.
|
|
|
|
|
|

|
EM BOUND TEAM
|
|
Editor-in-Chief; Rotation Tune-Up, COVID-19 Updates: Sree Natesan, MD (Duke University)
|
|
Clerkship Section Editor: David Gordon MD (Duke University)
|
|
SpotLight Section Editor: Moises Gallegos, MD MPH (Stanford University)
|
|
Wellness Corner Section & SoMe Editor: Al’ai Alvarez, MD (Stanford University)
|
|
EM Over Easy Editor: Andy Little, MD (AdventHealth)
|
|
Chief Advisor: Michelle Lin, MD (University of California, San Francisco)
|
|
|
|
|
|
|
|