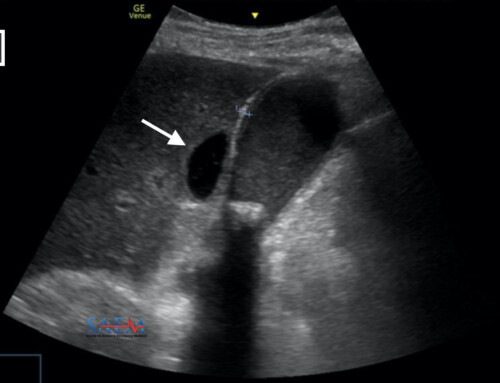
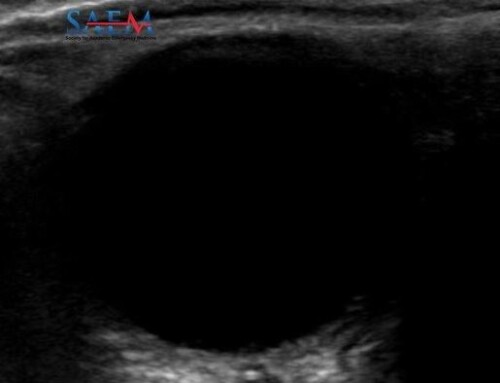
As bedside ultrasonography is becoming a staple in central line placement (especially of internal jugular lines), emergency physicians now can minimize complications, such as carotid artery puncture and a pneumothorax. Traditionally, the US probe is positioned along the short-axis of the IJ during the procedure (see right).
In an article published in Critical Care Medicine, the authors challenge providers to use the long-axis, rather than the short-axis view. Why, you ask? Because of the risk of posterior wall puncture of the IJ vein.
Study design
Using a life-like human torso mannequin, 25 EM residents placed ultrasound-guided IJ lines. All had attended a 3-hour didactic and hands-on session on the procedure. Also all had placed ultrasound-guided IJ lines previously in actual patients.
The residents used the short-axis U/S view of the IJ. During this procedure, one investigator tracked the resident’s needle using an endocavitary probe just inferior to the vascular probe. The convex shape of the endocavitary probe made it possible to visualize the soft tissue directly under the vascular probe.
The residents were asked to stop the procedure once they felt that the needle tip was in the middle of the IJ vein. The guidewire was not introduced.
The endocavitary probe tracked the needle course.
(image from Crit Care Med article)
IJ vein in long view with needle puncturing lumen
Main outcome measure
The incidence of posterior wall penetration, as defined as a 2nd venous wall penetration with an antecedent anterior wall penetration by the needle and needle shaft.
Results
At first glance, the study results were very surprising. I have always had great results with the short-axis view of the IJ for line placement.
- 16 of 25 residents (64%) accidentally penetrated the posterior wall while attempting to cannulate the IJ vein with a needle.
- For 6 of 25 residents (24%), the final position of the needle tip was posterior to the venous lumen.
- For 5 of 25 residents (20%), the final position of the needle tip was in the carotid artery
- More advanced training (r=-0.41) and degree of experience with ultrasound guided central lines (r=-0.54) were inversely correlated with posterior vein wall penetration.
Bottom line and thoughts
Overall, while this study brings up an interesting discussion about the best view for IJ line placement, I question the clinical significance of the study findings.
- The residents were not allowed to feed a guidewire to confirm successful IJ cannulation. For the 24% of residents who had positioned the needle tip posterior to the IJ lumen, I presume that the guidewire would not have been able to feed completely, if this were an actual patient. Consequently, the resident would have re-positioned the needle.
- If someone penetrated the posterior wall while trying to cannulate the IJ vein (64% incidence in this study), does this clinically matter if the needle and guidewire eventually end up in the IJ vein? I don’t think so.
- For the 20% of residents who had the needle tip in the carotid artery lumen, presumably the bright red nature or pulsatile flow of the blood return in an actual patient would have alarmed the resident (and attending!) that the needle was in the incorrect location and required repositioning.
While this study brings up an interesting complication of IJ line placement using the short-axis U/S view, the next step is to do this study in actual patients.
Words of caution
If you are thinking of using the long axis view of the IJ, start by finding the IJ using the short axis view. Keeping the IJ vein on the screen at all times, rotate the probe 90-degrees into the long axis view. Be sure that you are still looking at the IJ vein and not the carotid artery. Often on the long axis view, you can only see one vascular structure at a time. Be sure it’s the right one!
Also with the long axis view, try to keep your needle directed within the plane of the ultrasound. The needle easily can move in and out of the plane and thus disappear from the screen.
Reference
Blaivas M, Adhikari S. An unseen danger: Frequency of posterior vessel wall penetration by needles during attempts to place internal jugular vein central catheters using ultrasound guidance. Crit Care Med 2009; 37:2345–9.