Epistaxis is a common presentation to the emergency department (ED)1 that can be challenging and time consuming. Knowledge of the pearls, pitfalls, and troubleshooting tips around managing nosebleeds often can be the difference between a frustrating versus straightforward ED stay for patients. Use the EPISTAXIS mnemonic to help you remember these points.
Epistaxis is a common presentation to the emergency department (ED)1 that can be challenging and time consuming. Knowledge of the pearls, pitfalls, and troubleshooting tips around managing nosebleeds often can be the difference between a frustrating versus straightforward ED stay for patients. Use the EPISTAXIS mnemonic to help you remember these points.
Epistaxis Mnemonic
E xamine | Attempt to distinguish between anterior and posterior bleeding |
P ressure | Apply pressure over the nose with compression device or fingers |
I rrigate | Irrigate with warm water |
S ilver nitrate | Apply silver nitrate locally, if anterior vessel identified |
T ampons | Insert anterior nasal or posterior balloon tampons |
A frin | Oxymetazoline can be sprayed in the nose as part of conservative treatment or applied on tampon |
t X A | Apply TXA as gel or solution on tampon |
I nterventional radiology | Contact interventional radiology for embolization in conjunction with ENT surgeon |
S urgical consultation | Obtain an early ENT consult for severe or high risk bleeding |
Anatomy
Anterior bleeding
- Contributes to majority of cases
- Occurs at the watershed area known as Kiesselbach’s plexus
Posterior bleeding
- Contributes to severe cases
- Arises from branches of the sphenopalatine artery (rare cases involve the carotid artery)
Etiology
- Causes include direct trauma, nose picking, irritation, dryness
- Associated with bleeding dyscrasia, congenital or traumatic arterio-venous malformations, anticoagulation, neoplasm
- The majority of bleeding is self-limited and easily controlled.
Epistaxis Solutions in the ED
Recurrent or intractable bleeding has led to the development of management algorithms in the urgent care setting.2,3
Examine/Ensure secure airway
Attempt to visualize site of bleeding. Have patient gently blow nose to clear the clots. Obtain adequate lighting and use a nasal speculum, if available.
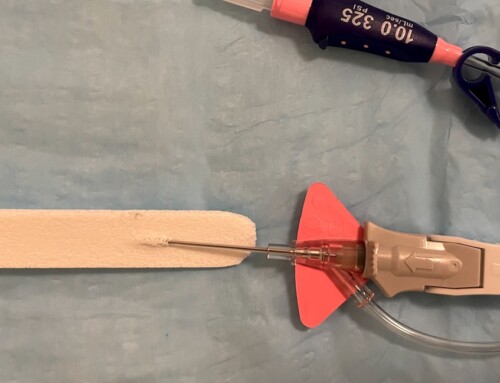
Pressure
As with any bleed, compression is key. Fatigue becomes an issue as patients tire of squeezing their nose. There are commercially available nasal compression clips, but in a pinch (get it?) you can create your own with tongue blades as demonstrated in this trick of the trade.
Irrigation
Irrigation of the nares can improve visibility. Warm-water irrigation has been demonstrated to facilitate hemostasis in posterior bleeds by causing mucosal edema that constricts vessels.4
Silver Nitrate/Cautery
If a bleeding anterior vessel is identified, an attempt at chemical or electrical cautery can be made. Silver nitrate sticks offer an easily accessible and efficacious option.5
Caution:
- Avoid bilateral septal cautery to prevent septal perforation.
- Carefully apply silver nitrate very focally on the mucosa being sure not to touch the skin, because it can accidentally burn and stain it (e.g. patient’s nasal ala) black.6
Tampons/Packing
Nasal tampons, often made of Merocel, are used for nasal packing. Patients may be pre-treated with topical lidocaine (2%) and/or oxymetazoline. Nasal tampons can be coated with bacitracin for lubrication before inserting along the nasal floor. Apply saline to expand the tampon. Tampons can also be inserted into the contralateral nostril for further compression.
Balloon catheter tampons provide an alternative option and can target posterior bleeding. They contain an internal balloon that is inflated for extra pressure. Such products have been shown to be easier to use and better tolerated; however, the efficacy is similar to Merocel tampons.7,8
If such balloon catheter tampons are not readily available for difficult cases of posterior bleeding, Foley catheters can be used.9 Insert a 10 or 12 French catheter so that the balloon lies in the nasopharynx. Inflate the balloon with 15 mL of saline, and then apply light forward traction on the catheter to tamponade the bleeding posterior vessels. If bleeding persists anteriorly or into the oropharynx, the balloon can be incrementally inflated up to 30 mL. Avoid inflation with air as the pressure can be lost over time.
Caution should be taken to avoid packing if there is concern for facial fractures.
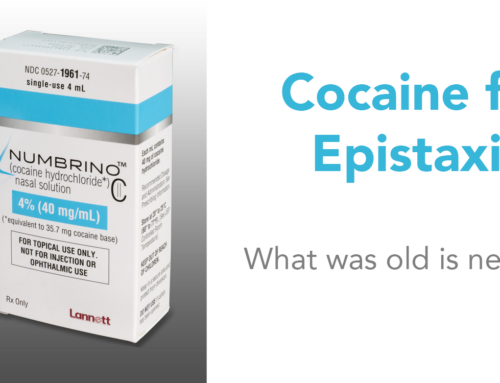
Afrin/Medication
Oxymetazoline (Afrin), a selective alpha-1 adrenergic receptor agonist and partial alpha-2 receptor agonist, has been shown to be an effective vasoconstrictor even for posterior bleeding.10 Use cautiously in hypertensive patients because elevated blood pressure may contribute to further bleeding. One trick is to apply oxymetazoline directly onto the tampons after insertion. This allows cotton to expand while also providing vasoconstriction.
TXA
The use of tranexamic acid (TXA) in epistaxis and mucosal bleeding has been a topic of interest. While research is equivocal, studies are promising regarding TXA application for nasal packing.11–13 The TXA dosing in Zahed et al.’s paper was 500 mg in 5 mL, applied on the nasal tampon.11
Interventional Radiology or Surgery
ENT consultation should be obtained in a timely manner for severe, refractory bleeding that may require intravascular embolization or surgical ligation.
Disposition
Patients with posterior epistaxis and packing should be admitted to the hospital for observation and ENT consultation.14 These patients may be at higher risk for bradydysrhythmias and recurrent bleeding, requiring surgery. Patients with anterior epistaxis who are hemostatic can be discharged home, assuming stable laboratory testing and vital signs. If they have nasal tampons in place, arrange ENT follow-up at 24-48 hours for re-evaluation and removal of tampons. The routine use of antibiotics to prevent toxic shock syndrome and sinus infections remains debated.
References
- Pallin D, Chng Y, McKay M, Emond J, Pelletier A, Camargo C. Epidemiology of epistaxis in US emergency departments, 1992 to 2001. Ann Emerg Med. 2005;46(1):77-81. [PubMed]
- Traboulsi H, Alam E, Hadi U. Changing Trends in the Management of Epistaxis. Int J Otolaryngol. 2015;2015:263987. [PubMed]
- Newton E, Lasso A, Petrcich W, Kilty S. An outcomes analysis of anterior epistaxis management in the emergency department. J Otolaryngol Head Neck Surg. 2016;45:24. [PubMed]
- Novoa E, Schlegel-Wagner C. Hot water irrigation as treatment for intractable posterior epistaxis in an out-patient setting. J Laryngol Otol. 2012;126(1):58-60. [PubMed]
- Shargorodsky J, Bleier B, Holbrook E, et al. Outcomes analysis in epistaxis management: development of a therapeutic algorithm. Otolaryngol Head Neck Surg. 2013;149(3):390-398. [PubMed]
- Maitra S, Gupta D. A simple technique to avoid staining of skin around nasal vestibule following cautery. Clin Otolaryngol. 2007;32(1):74. [PubMed]
- Badran K, Malik T, Belloso A, Timms M. Randomized controlled trial comparing Merocel and RapidRhino packing in the management of anterior epistaxis. Clin Otolaryngol. 2005;30(4):333-337. [PubMed]
- Singer A, Blanda M, Cronin K, et al. Comparison of nasal tampons for the treatment of epistaxis in the emergency department: a randomized controlled trial. Ann Emerg Med. 2005;45(2):134-139. [PubMed]
- Ho E, Mansell N. How we do it: a practical approach to Foley catheter posterior nasal packing. Clin Otolaryngol Allied Sci. 2004;29(6):754-757. [PubMed]
- Doo G, Johnson D. Oxymetazoline in the treatment of posterior epistaxis. Hawaii Med J. 1999;58(8):210-212. [PubMed]
- Zahed R, Moharamzadeh P, Alizadeharasi S, Ghasemi A, Saeedi M. A new and rapid method for epistaxis treatment using injectable form of tranexamic acid topically: a randomized controlled trial. Am J Emerg Med. 2013;31(9):1389-1392. [PubMed]
- Kamhieh Y, Fox H. Tranexamic acid in epistaxis: a systematic review. Clin Otolaryngol. 2016;41(6):771-776. [PubMed]
- Tibbelin A, Aust R, Bende M, et al. Effect of local tranexamic acid gel in the treatment of epistaxis. ORL J Otorhinolaryngol Relat Spec. 1995;57(4):207-209. [PubMed]
- Supriya M, Shakeel M, Veitch D, Ah-See K. Epistaxis: prospective evaluation of bleeding site and its impact on patient outcome. J Laryngol Otol. 2010;124(7):744-749. [PubMed]