Troponin testing is an important component of the diagnostic workup and management of acute coronary syndromes (ACS). The increasing sensitivity of troponin assays has lowered the number of potentially missed ACS diagnoses, but this has also created a diagnostic challenge due to a decrease in the specificity of the test. From 1995 to 2007, the limit of troponin detection fell from 0.5 ng/mL to 0.006 ng/mL (see below graph). Robert Jesse summed up this frustration with the following quote:
Troponin testing is an important component of the diagnostic workup and management of acute coronary syndromes (ACS). The increasing sensitivity of troponin assays has lowered the number of potentially missed ACS diagnoses, but this has also created a diagnostic challenge due to a decrease in the specificity of the test. From 1995 to 2007, the limit of troponin detection fell from 0.5 ng/mL to 0.006 ng/mL (see below graph). Robert Jesse summed up this frustration with the following quote:
When troponin was a lousy assay it was a great test, but now that it’s becoming a great assay, it’s getting to be a lousy test.
Image modified from 1
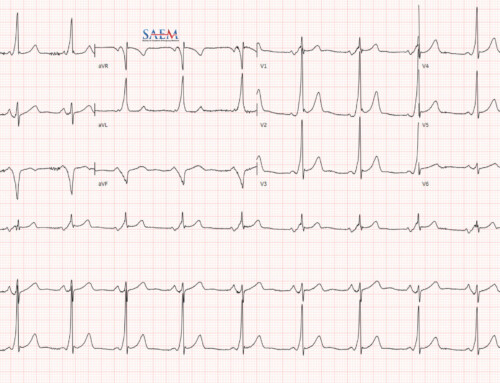
How good is ECG alone for diagnosis of acute myocardial infarction (AMI)? 2
- Specificity 97%
- Sensitivity 28%
- Due to the poor sensitivity of ECGs, cardiac biomarkers are also needed.
Does an elevated high sensitivity troponin (hsTn) mean acute coronary syndrome (ACS)?
- hsTn can be found circulating in the plasma as a result of any transient ischemic or inflammatory myocardial injury, such as cardioversion, CHF, aortic dissection, HOCM, tachyarrhythmia, myocarditis/pericarditis 1
- Non-cardiac causes of elevated hsTn include: PE, renal failure, SAH, sepsis, burns, and extreme exertion (i.e. marathons) 1
What should a provider do with troponin elevation from non-ACS etiologies? 3
- Unfortunately, little data is available on management of these patients
- There is data evolving on elevated Tn levels in conditions such as CHF, PE, sepsis, and renal failure
- There is a proposed algorithm currently from the best evidence available (has not been validated):
How often is serial troponin testing needed with hsTn to rule out acute MI (every 2, 4, 6, or 8 hours)?
- 1/5 of patients with normal hsTn at presentation will be diagnosed with AMI on repeat testing 4
- The National Institute for Health and Clinical Excellence (NICE) Guidelines recommend measuring Tn on admission and 10 – 12 hours after the onset of symptoms (This needs to be updated, due to current use of hsTn testing) 2
- Most recent guidelines from Global Task Force state Tn testing should be obtained at admission and at 3 – 6 hours after admission, irrespective of the timing of the onset of symptoms 4
- Lower sensitivity Tn requires at least 6 hours between time of initial lab and repeat Tn to see a conclusive increase to rule in AMI 1
- High sensitivity Tn requires only 2 to 3 hours between time of initial lab and repeat Tn to see a conclusive increase to rule in AMI 1
- A normal hsTn at 3 hours has a NPV of 99% in excluding AMI 2
- Dr Louise Cullen et al have recently published a paper:5
- 1,635 patients with 30 day follow up for Major Adverse Cardiac Events (MACE)
- Non-ischemic ECG, TIMI of 0, and negative hsTn (0 and 2 hours): 0% MACE with Sens 100%, Spec 23.1%, NPV 100%
- Non-ischemic ECG, TIMI of ≤1, and negative hsTn (0 and 2 hours): 0.8% MACE with Sens 99.2%, Spec 48.7%, and NPV 99.7%
- Conclusion: Early discharge strategy utilizing a hsTn assay, TIMI ≤1, and non-ischemic ECG can safely decrease observation periods and admissions in approximately 40% of patients with suspected ACS
- Current best EBM: Serial sampling of hsTn at 0 and 2 hours is essential to permit the safe rule-out of AMI and to minimize misdiagnosis in patients with elevated hsTn (Another case of guidelines being behind)
What is considered a “significant change” in hsTn levels? 4
- According to the European Society of Cardiology (ESC):
- Increase of ≥20% if first Tn elevated, or
- Increase of ≥50% in patients with small initial Tn elevations
Conclusion
hsTn is the preferred biomarker for the diagnosis of AMI, but remember that conditions other than AMI may cause acute and chronic elevations.