Point-of-care ultrasound (PoCUS) has become an essential skill that emergency medicine (EM) residents learn during their training [1]. Accordingly, most EM programs schedule a block early in residency dedicated to obtaining and interpreting high-quality PoCUS images. Likewise, the ability to efficiently diagnose and manage acute cardiovascular pathologies is a critical aspect of EM, and most EM residents also rotate on a cardiology service to develop these skills. Despite evidence that PoCUS improves the ability of both cardiologists and non-cardiologists to quickly diagnose cardiac disease at the bedside, integration of this relatively novel technology on cardiology services is often limited by lack of PoCUS availability as well as lack of a convenient platform to share recorded images [2]. Equipping EM residents on cardiology rotations with a portable, handheld ultrasound (US) system (Figure 1. Philips Lumify handheld US system with tablet) can enhance the learning of echocardiography acquisition and interpretation while simultaneously providing cardiology teams with clinically actionable information [3]. In addition to improving patient care, performing and interpreting PoCUS from the lens of a cardiologist is a simple yet innovative way to solidify the skills that are crucial to becoming an excellent bedside echocardiographer.
The Innovation
Providing a handheld US system to EM residents rotating on cardiology services such that US images can be captured and shared in real-time within the cardiology team.
The Learners
This innovation targets EM residents but also benefits others rotating on the cardiology service including internal medicine residents, physician assistants, and medical students. Utilizing the handheld US system, echocardiography images are obtained as directed by the attending cardiologist. These images are stored on the US device and can then be interpreted in the clinical context of the case in discussion with the full cardiology team.
Equipment
- Portable, handheld US transducer
- Tablet or phone to view, store, and share images
- US gel and disinfectant wipes

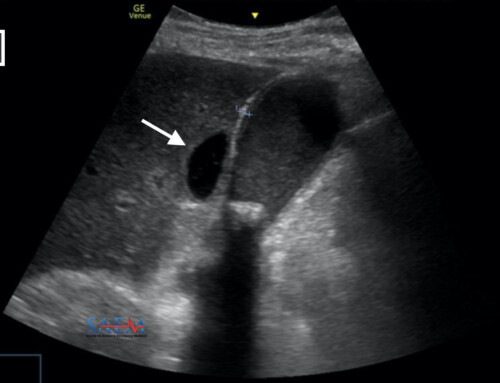
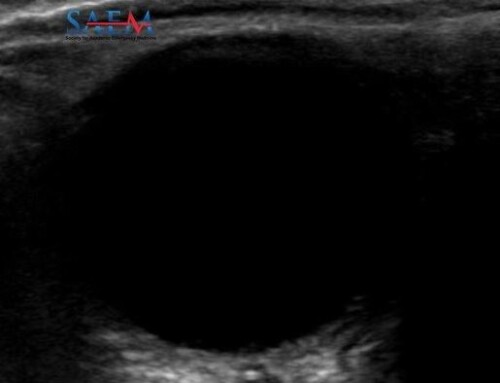
Figure 2. Sample bedside echocardiology captured by a PGY-2 resident with a Philips Lumify transducer. A. Parasternal long view. B. Parasternal short view. C. Apical four-chamber view. D. Subxiphoid view.
Description of the Innovation
This innovation involves equipping EM residents rotating on the cardiology service (a PGY-2 rotating for one month at our program) with a portable, handheld US system. This device is used to perform bedside echocardiology for consults in the emergency department and inpatient wards. This not only allows active echocardiography learning by the resident but also allows the cardiology team to follow day-to-day changes in a patient’s cardiac function. The system can also be used for procedural guidance as needed. Moreover, if the attending cardiologist is not able to come to the bedside for the initial consultation, the tele-sonography function allows real-time feedback and guidance with regard to image acquisition. For our novel project, we utilized a Philips Lumify phased array transducer attached to a simple tablet.
Lessons Learned
- Our project was designed to provide longitudinal learning by allowing PGY-2 residents to build upon skills developed during a dedicated PGY-1 PoCUS rotation. The cardiology service is an ideal PoCUS training environment as residents work closely with experienced cardiologists who can provide direct feedback on image quality and interpretation. In addition, the rotation affords more time for dedicated teaching than a typical high-volume emergency department shift.
- This project also provides the cardiology service with clinically useful information that has the potential to change patient management. For instance, EM residents can frequently obtain high-quality echocardiography images before comprehensive transthoracic or transesophageal echocardiography studies can be completed. In our institution, we have found this to be especially helpful in the setting of COVID-19 as there is often a delay in obtaining comprehensive echocardiography.
- For rotating EM residents, this project also allows the unique opportunity to follow patients’ status throughout their hospitalizations, with opportunities to frequently re-image and observe the cardiovascular response to interventions such as diuresis, vasopressor support, or procedures like pericardiocentesis. While serial PoCUS exams are sometimes difficult to perform in the emergency department, such longitudinal exams can easily be acquired and compared on the cardiology service.
Educational Theory
This project is rooted in visual and procedural learning and follows a model proposed by K. Anders Ericsson in which deliberate practice and direct feedback from experts are key components [4]. Ericsson’s model has previously been applied to PoCUS training for EM residents with encouraging results [5]. For individuals with an intermediate level of echocardiography experience, such as PGY-2 EM residents, this model creates an ideal framework for honing the skill. Our clinical environment provides opportunities for repetition and refinement of technique as well as direct observation and feedback from experts. We believe that giving EM residents the ability to efficiently perform bedside echocardiography and interpret these data in real-time with attending cardiologists is a highly effective mode of learning.
Closing Thoughts
Overall, both EM residents and our hospital’s cardiologists have provided positive feedback on this initiative. It has enhanced resident learning of echocardiography skills and has been particularly useful in instances where comprehensive echocardiography is not rapidly available. In these instances, our PoCUS exams have helped guide clinical management. We hope to continue this project to further improve our residents’ PoCUS skills.
References
- Akhtar S, Theodoro D, Gaspari R, et al. Resident training in emergency ultrasound: Consensus recommendations from the 2008 Council of Emergency Medicine Residency Directors Conference. Acad Emerg Med. 2009;16 Suppl 2:S32-6. PMID: 20053207
- Kimura BJ. Point-of-care cardiac ultrasound techniques in the physical examination: Better at the bedside. Heart. 2017;103(13):987-994. PMID: 28259843
- Farsi D, Hajsadeghi S, Hajighanbari MJ, et al. Focused cardiac ultrasound (FoCUS) by emergency medicine residents in patients with suspected cardiovascular diseases. J Ultrasound. 2017;20(2):133-138. PMID: 28593003
- Ericsson KA, Krampe RT, Tesch-Römer C. The role of deliberate practice in the acquisition of expert performance. Psychological Review. 1993;100(3):363-406.
- Hayward M, Chan T, Healey A. Dedicated time for deliberate practice: One emergency medicine program’s approach to point-of-care ultrasound (PoCUS) training. CJEM. 2015;17(5):558-561. PMID: 26030268
Disclosures
The authors have no financial disclosures. Dr. Nagdev is associated with Ondas de LatinoAmerica which has received an educational grant from the Philips Foundation to purchase ultrasound systems and educate Latin American ED sonographers.