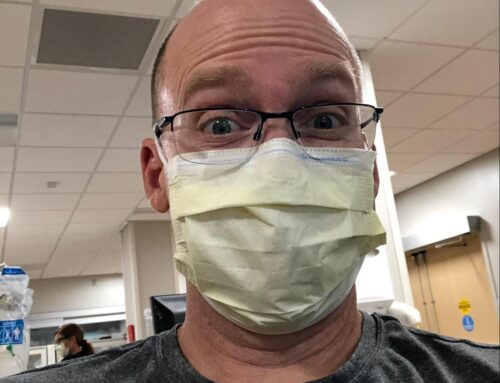
Dr. Rob Woods (@robwoodsuofs) is an individual that is truly committed to self-improvement and, in terms of wellness, he has exceeded. Currently, he is the program director of the University of Saskatchewan FRCPC EM Program, Medical Advisor to Ground Ambulance Services, and a STARS (HEMS) Transport Physician. How he excels in all these jobs and still has time to be known as a loving father and husband, amazing Program Director, and CrossFitter is incomprehensible! But it may have something to do with the fact that he has mastered time management. A great competitor on and off the field, Dr. Woods is never afraid to show his competitive side, which always makes things a bit more fun! Here’s how he manages to stay healthy in EM!
- Name: Rob Woods, MD MMEd FRCPC

- Location: Saskatoon, Saskatchewan
- Current job(s): Father of 2, Husband, Adult and Pediatric Emergency Physician. Program Director University of Saskatchewan FRCPC EM Program, Medical Advisor of the Ground Ambulance Services – Saskatoon Health Region, STARS Transport Physician
- One word that describes how you stay healthy: Time Management
- Primary behavior/activity for destressing: Exercise and ‘talking it out’ with my support network.
What are the top 3 ways you keep healthy?
- Exercise. Exercise is one of the most important things you can do to stay healthy. Even if I keep my time management in check and there is time to exercise, I struggle to motivate myself to do it on my own. My attempts to ‘work out’ on my own in the past never lasted long; it was tough to motivate myself to go to the gym, and when I got there, the intensity of my workout was often limited. For that reason I rely on group activities to ensure I am exercising regularly. I thrived in team sports in high school and university, but being a shift worker takes a major toll on your ability to commit to a team that plays at the same time each week. I still play basketball, but I can only make about 70% of the games. Thankfully I have teammates who allow me to do this. I have also been going to CrossFit group classes for the past 4 years. I love that I can do a scheduled group activity in the daytime hours when my kids are at school and I am often not working a shift. It motivates me to fit it in, and to give it my best when I am there. The social aspect makes it a lot of fun, and it has given me a new social/support network.
- Know your canaries. Figure out the warning signs that your wellness is in danger. My canaries are lack of exercise, then minimal time with my spouse, then excessive caffeine and sugar to deal with fatigue, and finally poor performance and a lack of excitement about work. I know I’ve probably taken on too much when I haven’t exercised for a week, my wife and I haven’t had a date for a while, and I’m reaching for that can of Coke. If I am driving to work and dreading being there, or each day it seems like I am just putting out fires, I know it’s time for me to search out someone in my support network and figure out where things broke down.
- Time Management. I get a lot of satisfaction out of work and often wish there were more hours in a day. I have yet to have a day where I had Emergency Medicine all figured out. The possibilities to try and make my specialty and practice better are endless. I know I can only do so much, so I make sure I have one day every month booked in my home office. It’s my ‘scheduled day to schedule’ and look after important maintenance tasks. This advanced planning makes it easy to confidently say ‘no’ to new things if I know that my schedule is filled up. I believe it’s important to see things through to completion if I take them on so this helps me to prevent point #2 from happening.
What’s your ideal workout?
I love anything with competition. I find competing against friends or the stakes of a sporting event to be a lot of fun. It allows me to really focus on the activity and take a true mental break from the other stressors in my life. I can find a way to make anything into a competition – just ask my friends and family.
Do you track your fitness? How?
I keep track of how often I exercise. My gym membership covers me for 10 classes per month, and I know I am doing well if I get charged for an extra class. If I get 7-8 in a month, that’s great. I play on 2 basketball teams, so if I make one game each week during the season that’s great, and if I make 2 it’s fantastic! In the summer I spend lots of time at the lake exercising outside.
How do you prepare for a night shift? How do you recover from one?
Preparation: For late evening and night shifts, I need to make sure I ‘get tired’ so I can pre-sleep effectively. Intense exercise followed by a good meal makes conditions perfect for a nap. I wake up at least an hour before I start my shift so I am mentally ready to work. You can only effectively do so much in a day so if I have an evening shift, and an afternoon meeting prior to it, the morning is low key. If I try to clean out my email, or work on a presentation that morning, half way through my shift I am mentally and physically fatigued, and can not give my best to my patients.
Recovery: After a late evening shift I find I am too wound up to sleep right away so I have a snack, watch some TV for 30-45 minutes, THEN go to bed. That way I fall asleep right away. After a night shift I try not to sleep too long (usually until noon or 1), then have a low-key day and try to stay up until my kids go to bed. That helps me to switch back to days as quickly as possible so I can be helpful to my wife.
How do you avoid getting “hangry” (angry due to hunger) on shift?
I try to pack easy to eat health snacks. Correction: my wife ensures I pack healthy snacks. Fruit (dried or fresh), bag of veggies, nuts, and protein bars all fit the bill. When there are treats in the department, I do indulge.
How do you ensure you are mentally in check?
Pre-shift: Show up a few minutes early, find the phone/pager, and put my numbers (department cellphone and pager) on the whiteboard so people can track me down. Then I scan the patient list to see how many patients are in the waiting room and how many are boarded to determine if I need to do some admin work prior to seeing patients or not. Finally, I meet with my learner and determine our goals. By the time I step into a patient’s room, I have a global plan for the shift and I can do my best to focus on the patient at hand.
On shift: I always keep track of my patient list and the department. My group is salaried, so I can shape my shift to optimize departmental flow without it affecting my income. As I move through the shift I try to ensure I do what’s best for the overall flow of patients. If there are lots of patients in beds to be seen, I go for it. If there are lots of boarded patients I do frequent re-assessments to ensure efficient discharges. Near the end of the shift I strategically pick up patients that are unlikely to be handed-over so the next physician can start seeing patients.
Post-shift: Following an evening shift I like to grab a drink/snack with your colleague +/- learner to unwind. After a day shift, I head home to see my family.
What are the biggest challenges you face in maintaining a longstanding career in EM? How do you address these challenges?
Working at multiple sites allows me to escape from the challenges of a particular site. For example, one of our sites is often overcrowded making it logistically challenging just to see patients. The other primary site has a high proportion of marginalized patients which can make it emotionally challenging. Working at both minimizes these effects. Adding shifts at the Peds ER adds another dimension of patient variety for me.
Developing a niche area of expertise in education and administration has helped me to decrease my clinical time a bit in exchange for additional 9-5 work. Shift work can isolate me from my family and social commitments and doing only clinical would have me spending 70% of my time working before 9 or after 5. Currently 25% of my work is a mix of education and administration. In addition, having a niche of expertise provides an exit strategy from clinical work. You can slowly migrate into your niche area, and decrease your clinical time.
Having a support network to de-stress is important. I have about 8 EM physician colleagues, and most importantly my wife, who I ‘vent’ to from time to time about aspects of my career that I find challenging. It’s good to have the trusting ear to allow you to have your emotional and irrational catharsis. Once that’s out, I can go forward with a balanced perspective on your stresses and challenges.
Best advice you have received for maintaining health?
‘Everything in moderation’
Gluten is not the enemy, and you can’t feed the world on paleo diets. Training to be an elite athlete is for some, but the risk of injury and resultant inactivity is high. Eat well most of the time, exercise regularly most of the time, and don’t get too stressed about it. Work hard, and find ways to make health care better for your patients, but not at the expense of your own physical and mental health. The rest of the work will look after itself.
Who would you love for us to track down to answer these questions?
Kathryn Dong
Marilyn Innes
Erica Dance