Welcome to another ultrasound-based case, part of the “Ultrasound For The Win!” (#US4TW) Case Series. In this peer-reviewed case series, we focus on real clinical cases where bedside ultrasound changed management or aided in diagnoses. In this case, a 55-year-old man presents with acute-onset chest pain.
Case Presentation
A 55-year-old man walks into your Emergency Department with a complaint of left-sided chest pain. He reports walking his dog outside 1 hour prior to arrival in the ED when he developed sudden-onset of crushing chest pain. His past medical history includes hypertension and hyperlipidemia, but he denies a prior known history of coronary artery disease. He took aspirin and his wife’s nitroglycerin without relief. He acknowledges associated shortness of breath. On physical examination, you observe a middle-aged, diaphoretic, and overweight man. His heart sounds are regular without murmurs, and his lungs are clear to auscultation bilaterally. Extremities are warm, with no edema.
Vitals
BP 115/75 mm Hg
P 76 bpm
RR 23 respirations/min
O2 97% saturation on room air
T 97.4 F
Differential Diagnosis
- Acute Coronary Syndrome
- Aortic Dissection
- Pneumothorax
- Pulmonary Embolism
Given the patient’s concerning symptoms, the Emergency Physician performed a bedside echocardiogram while awaiting an EKG.
Point-of-care Ultrasound

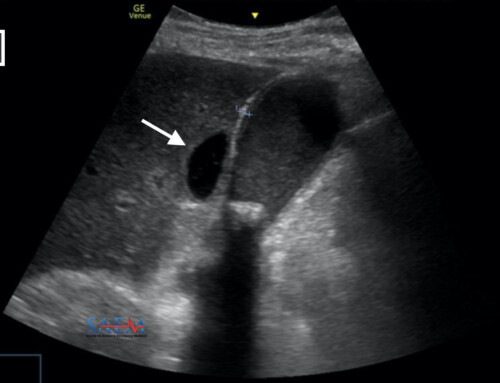
Figure 1. Parasternal Short Axis (PSSA) view revealing hypokinetic septal and anterior segments

Figure 2. Identification of areas of the left ventricle (LV), “SALPI”: Septal (S), Anterior (A), Lateral (L), Posterior (P), Inferior (I). Right ventricle (RV) is also seen

Figure 3. Electrocardiogram (EKG) concerning for anterior ST-elevation myocardial infarction (STEMI)
The patient’s symptoms along with the EKG and correlating bedside echo were concerning for an acute MI, and the cardiac catheterization lab was activated.
Ultrasound Image Quality Assurance (QA)
The ability to identify regional wall motion abnormalities (RWMAs) on echocardiography is considered an advanced but important skill for an Emergency Physician to have. For further discussion on proper probe orientation and various cardiac views, please refer to a prior Ultrasound for the Win! Case.
Arguably the most useful view to identify RWMAs is the parasternal short axis view, with the probe marker oriented to the patient’s right hip, producing an image that cuts through the left ventricle (LV) in its short axis (Figure 4). Seen on this clip is normal concentric contraction and adequate muscle thickening throughout all regions of the left ventricle.

Figure 4. Normal parasternal short axis (PSSA) view of the heart
Using the PSSA view, regions of the left ventricle can be identified using the mnemonic “SALPI” (Figure 2). RWMAs are identified by visualizing areas of hypokinesis or akinesis. More specifically, looking at how well the cardiac muscle thickens during systole is helpful in identifying wall motion abnormalities. Once RWMAs are identified, these can generally be attributed to ischemia of a coronary vessel(s) (Figure 4, Table 1). In the images obtained in this case, the septal and anterior portions are hypokinetic correlating to ischemia of the left anterior descending (LAD) artery.

Figure 5. Generalized correlation of left ventricular wall regions with coronary vessels; left anterior descending (LAD), circumflex (Cx), and right coronary artery (RCA)
Table 1. Correlation of regional wall motion abnormality to ischemia of a coronary vessel
| Region of Left Ventricle | Coronary Vessel |
| Septum; Anterior; Apex | Left anterior descending (LAD) |
| Lateral | Circumflex (Cx) |
| Inferior | Right coronary artery (RCA) |
Disposition and Case Conclusion
The patient was emergently taken to the cardiac catheterization lab, where he was found to have a complete acute occlusion of the proximal LAD. His troponin I eventually came back, elevated at 0.16 ng/mL. He underwent a successful thrombectomy and stenting, and was observed in the hospital for 72 hours. He has since been discharged and is doing well!
More than 5 million people present to emergency departments with chest pain1, and it is important to be able to risk stratify these patients and identify those with acute coronary syndrome (ACS). However, this diagnosis remains a difficult, resource and time-intensive task with a high potential morbidity and mortality.
While the electrocardiogram (EKG) in this case was diagnostic of a STEMI, this is often not the case for patients who present to the ED with acute coronary syndrome. While an EKG is the most widely used screening tool, it is only diagnostic in the minority of cases.2 In fact, the initial EKG is diagnostic for predicting cardiac events including acute myocardial infarction and/or revascularization in only 40% of patients, while the sensitivity for echo is much higher at 90%1. The reason behind this lies in the concept that EKGs are appropriate for identifying infarction, whereas an echo can identify ischemia without infarction, since necrosis is not needed to cause wall motion abnormalities.
The usefulness of an echo to identify regional wall motion abnormalities cannot be understated; studies have found that RWMAs are found in 90-100% of patients with a transmural infarction, and 86% of patients with non-Q-wave myocardial infarction.2 However, the utility of the bedside echo lies not only in identifying cases of ACS, but also in identifying patients who are at low risk for ACS. A normal echo performed during active chest pain is a strong predictor of a non-ischemic etiology.3 Additionally, alternate causes for chest pain, such as cardiac tamponade or a pulmonary embolism, may be evident on the echocardiogram.
Emergency Physicians have the unique opportunity to perform a bedside echocardiogram immediately upon a patient’s presentation. In the acute setting where “time is muscle”, sending a patient to get an echo performed by a cardiologist or technician may not be a viable option. A study by Kerwin et al. found that after a brief training video, Emergency Physicians can identify RWMAs with 87% accuracy.4 The ability to perform a bedside echo, in conjunction with the clinical scenario and other diagnostic tests, allows Emergency Physicians to quickly identify patients with a non-diagnostic EKG who may benefit from urgent cath lab activation. It is important to note that RWMAs have been shown to be the first clinically evident sign of acute cardiac ischemia, before EKG and even chest pain.5
There are caveats to identifying RWMAs on echo; namely patients with prior/old lesions, obtaining adequate cardiac views, and patients with existing significant left-ventricular dysfunction. In these cases, however, patients are at higher risk for ACS and would likely benefit for further investigations.
In summary, in patients with concern for ACS and a non-diagnostic EKG, a bedside echo performed by the Emergency Physician can be a useful diagnostic tool that can be used to supplement the clinical scenario.
Take Home Points
- Bedside echocardiography can be a useful supplemental diagnostic tool to risk-stratify patients who present to the Emergency Department with chest pain.
- Regional wall motion abnormalities on echo is the earliest clinically evident sign of ischemia and is more sensitive for predicting cardiac events than both EKG changes and onset of chest pain.
- Caveats to the bedside echo to identify regional wall motion abnormalities include prior infarcts and inadequate cardiac views.