Welcome to another ultrasound-based case, part of the “Ultrasound For The Win!” (#US4TW) Case Series. In this peer-reviewed case series, we focus on a real clinical case where bedside ultrasound changed the management or aided in the diagnosis. In this case, a 39-year-old female with history of lupus presents with chest pain.
Case Presentation
A 39-year-old female with history of lupus presents to the Emergency Department via EMS for evaluation of chest pain. Of note, she was recently discharged from the hospital for pneumonia with an exudative pleural effusion. Per EMS report, she was noted to be hypotensive with systolic pressures in the 70s, and two peripheral IV’s were started with IV fluids running. A rhythm strip from the field reveals a narrow complex tachycardia.
On examination, the patient is distressed, tachypneic, and has distended neck veins.
Vitals
BP 90/60 mm Hg
P 146 bpm
RR 31 respirations/min
O2 96% on non-rebreather
T 36.8 C
Differential Diagnosis
- Acute Coronary Syndrome
- Arrhythmia
- Pericardial Tamponade
- Pleural Effusion
- Pneumonia
- Pneumothorax
- Pulmonary Embolism
Point-of-care Ultrasound
A patient who presents to the ED with chest pain in shock has a wide differential, several of which are noted above. The rapid use of one of many bedside ultrasound-guided protocols (e.g. RUSH, ACES) can be used to aid in narrowing your differential and finding potential reversible causes of shock. These protocols usually combine a few focused exams, including echo, IVC, thoracic, and aorta. In this case, an echocardiogram was performed first, which revealed the following:
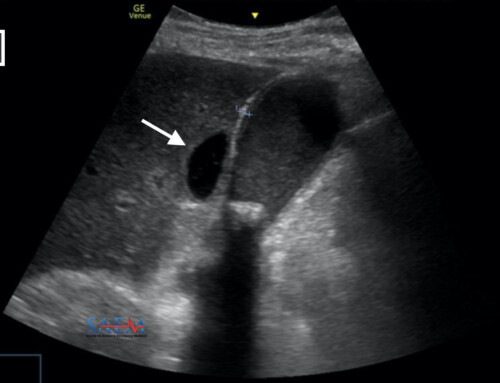
The bedside echocardiogram reveals a large circumscribed pericardial effusion with hemodynamic compromise and pericardial tamponade, including right atrial systolic collapse and right ventricular diastolic collapse. In addition, a scan of the IVC (not shown) was found to be plethoric with minimal respiro-phasic variation, consistent with the patient’s presentation of obstructive shock.

Parasternal Short Axis view of the heart with large pericardial effusion (blue arrow) with right ventricular (RV) collapse. Also seen is the left ventricle (LV).
A pericardial effusion appears as an anechoic stripe adjacent to the pericardium, which is usually circumferential, and should extend anterior to the descending aorta (visualized posterior to the left atrium on a parasternal long axis view).1 However, if a loculated pericardial effusion is present, as is the case with this patient, it may not be evident on all views and may be missed if multiple views are not obtained. This reinforces the importance of obtaining multiple views when performing a bedside echocardiogram.
Another common pitfall includes mistakenly identifying a pleural effusion as a pericardial effusion. In contrast to pericardial effusions, pleural effusions will collect posteriorly to the descending aorta. The following image, of another patient with both pericardial and pleural effusions, illustrates this concept.

Parasternal Long Axis View of the Heart. A pericardial effusion (pink) is seen anterior to the descending thoracic aorta (Ao), whereas a pleural effusion (blue) is seen posterior to the Ao. LA=left atrium, RV=right ventricle, LV=left ventricle.
Lastly, another pitfall is mistaking an epicardial fat pad with a pericardial effusion – an epicardial fat pad will usually be located only anteriorly, and is not completely anechoic.
Ultrasound Image Quality Assurance (QA)
An important aspect of ultrasound is appropriate and optimal image acquisition. The bedside echo shows optimal gain and depth. Another great aspect of this bedside echo is the capture of several views (apical-4-chamber, parasternal long axis, and parasternal short axis views of the heart, respectively). While a small effusion may be noted in the apical 4-chamber and parasternal long views, the loculated effusion in this particular patient is only really marked in the parasternal short axis! This highlights the importance of obtaining multiple views when performing an echo, and a general rule to follow for all ultrasounds you perform.
For further discussion on obtaining optimal cardiac views, and differences between ED and Cardiology probe-to-screen conventions, refer to a previous Ultrasound For the Win Case.
Disposition and Case Conclusion
Patients who present to the ED with shock require expeditious care and treatment. The use of bedside ultrasound is critical in narrowing the differential and providing high-quality care. This case highlights the role of resuscitative ultrasound in guiding the clinical pathway and management of the patient.
In this case, the cath lab was activated for emergent pericardiocentesis within minutes of obtaining the bedside echocardiogram. A formal echo obtained in the cardiac suite confirmed the initial focused echo findings: a loculated anterior pericardial effusion was noted. Due to the loculated nature of this effusion, pericardiocentesis was difficult, and the patient was taken emergently to the OR for a pericardial window, pericardial stripping, and a total pericardiectomy. She was discharged in good condition 10 days later from the hospital. The cause of the initial effusion was thought to be lupus related.
While bedside echocardiography can accurately visualize pericardial effusions, it is important to remember that this does not mean the patient has cardiac tamponade. Furthermore, the size of a pericardial effusion does not predict tamponade or hemodynamic instability; a large effusion may be chronic and the patient may be asymptomatic, and a small effusion may cause tamponade and hemodynamic instability.
Echocardiographic signs of tamponade or impending tamponade include RA collapse in systole and/or RV collapse in diastole. This can be fairly easily obtained and visualized with M-mode (which represents motion of structures over time) in a parasternal long axis view of the heart with the M-line transecting through both the RV and mitral valve. For further discussion on this as well as a great image, please refer to an excellent article by Nagdev and Stone.2 Another echocardiographic sign of tamponade is visualization of a plethoric IVC with minimal respiro-phasic variability.2 While a plethoric IVC is non-specific and can be seen in other scenarios such as fluid overload, pulmonary embolism, and right heart strain, it can be helpful in the right clinical context.
Take Home Points
- The use of resuscitative bedside ultrasound is critical in guiding care in patients with shock.
- Be aware of common pitfalls of pericardial effusion when assessing for pericardial effusions:
- Mistaking a fat pad or pleural effusion as a pericardial effusion
- Missing a localized, loculated pericardial effusion
- Not all pericardial effusions cause cardiac tamponade.
- Echocardiographic evidence of cardiac tamponade includes right atrial collapse during systole, right ventricular collapse during diastole, and a plethoric IVC with decreased respiro-phasic variation.
*Note: All identifying information and certain aspects of the case have been changed to maintain patient confidentiality and protected health information (PHI).