Welcome to another ultrasound-based case, part of the “Ultrasound For The Win!” (#US4TW) Case Series. In this peer-reviewed case series, we focus on real clinical cases where bedside ultrasound changed management or aided in diagnoses. In today’s case, a 74-year-old woman presents to the Emergency Department with painful right arm paresthesias.
Case Presentation
A 74-year-old female with history of atrial fibrillation presents to the Emergency Department with 45 minutes of painful right arm tingling that are now resolving. She has been off warfarin for the past 2 weeks for knee surgery. She reports no right arm weakness or color change. She reports left shoulder pain 12 hours prior to presentation. No complaints of shortness of breath or chest pain.
Vitals
- BP 150/52 mm Hg left arm, 30/- mm Hg right arm (automatic BP cuff)
- P 96 bpm
- RR 18 respirations/min
- O2 94% on room air (left arm); 85% on room air (right arm)
- T 37.3 C
Physical Examination
- Right arm:
- No palpable radial or brachial pulses
- Normal strength and sensation
- Capillary refill 3 seconds
- Left arm:
- Normal radial and brachial pulses
- Normal strength and sensation
- Capillary refill <2 seconds
- Lower Extremities:
- Normal and symmetric bilateral femoral, posterior tibial and dorsalis pedis pulses.
- Normal strength and sensation bilaterally
- Cardiac and lung exams:
- Normal
Differential Diagnosis
- Arterial thromboembolism of right arm
- Stroke/cerebrovascular accident
- Thoracic aortic dissection
Further Studies
Labs revealed a subtherapeutic INR of 1.5. A CT angiogram of the chest and abdomen was performed due to concern for possible dissection versus thromboembolism, and revealed:
- No evidence of thoracic aortic dissection
- Normal right brachiocephalic artery seen to axillary artery
- Multiple areas of atherosclerotic disease
Point-of-care Ultrasound
Given the ongoing concern for possible thrombo-embolic disease, a point-of-care ultrasound of the right upper extremity was performed:


Axillary artery visualized with pulsations in B-Mode (left) and with color doppler (right)

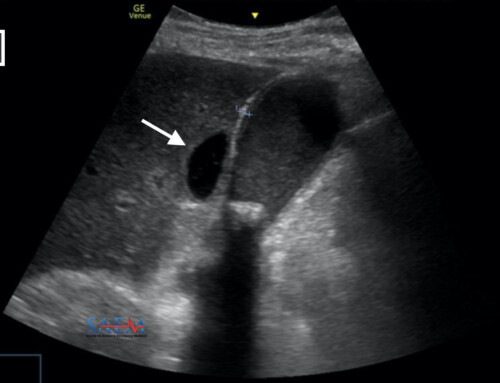
With significant external compression with the probe, a visualized thrombus (blue arrow) is seen within a non-compressible brachial artery

Ultrasound Image Quality Assurance (QA)
Ultrasound evaluation of the vascular system in the extremities is performed using the high-frequency linear transducer. It is important to optimize positioning of the patient when performing any point-of-care ultrasound; when evaluating the vessels of the upper extremity, the patient should be supine, with the shoulder abducted and externally rotated, and elbow flexed.1 Evaluation should include vessel identification, and assessment of vessel compressibility and blood flow. When using B-mode (normal gray scale) the angle of the probe in relation to the vessel should be as close to 90 degrees as possible, which will improve the definition of the vessel as well as the clot. Color doppler is used to assess direction of flow and can help to differentiate vascular from non-vascular structures such as nerves, lymph nodes, and bursae.
The use of color doppler is based on measurements of movement. Specifically in this case, it was used to measure the movement of blood in vessels, which is processed as a color flow display. A common misconception is that red is arterial flow, and blue is venous flow, however this is not necessarily always the case. In fact, by default, red is simply indicative of flow moving towards the probe, and blue is indicative of flow moving away from the probe. This is important to note as the doppler ultrasound beam must be aligned to the direction of flow (angle of insonation), or more parallel to the flow (typically <60 degrees), as opposed to perpendicular to the flow. The figure below illustrates this concept.

Effect of transducer position (angle of insonation) on color doppler signal interpretation. Image courtesy of Dr. Mike Mallin.
Also keep in mind your scale when using color doppler. The higher the flow state (e.g. an artery), the higher your scale should be. If the scale is set too low (as is the case in these clips), you will see more artifact including aliasing, which is an artifact where the color signal “folds over” and falsely appears to be reversing flow. In general when using color and pulsed wave doppler, the scale should be optimized to minimize aliasing, and the gain should be turned up until color artifact is seen, then turned down just below that point.

Use of a low scale (4 cm/s in this case) on a high-flow vessel can produce an aliasing artifact, falsely appearing as reversal of flow
Disposition and Case Conclusion
Given the patient’s symptoms and point-of-care ultrasound findings of a non-compressible right brachial artery with visible thrombus, a heparin bolus and infusion were initiated. Vascular surgery was emergently consulted, and the patient was taken for emergent right brachial artery thrombectomy with removal of a large subacute thrombus with restoration of normal perfusion in her arm. She was discharged home the next day on enoxaparin as a bridge back to warfarin.
Point-of-care ultrasound for evaluation of arterial thrombus is an advanced skill, and there is limited evidence on its use by emergency physicians. If there is a concern for arterial thromboembolism in a patient, a vascular surgeon should be consulted given the emergent nature of the process. Revascularization of an ischemic limb within 12 hours has an amputation rate of 6%, and rises to 20% at 24 hours.1 Given the need for timely diagnosis, point-of-care ultrasonography can be a beneficial skill for the emergency physican to have, as it can potentially shorten both time-to-diagnosis and time-to-embolectomy.
Take Home Points
- While there is limited evidence on the use of point-of-care ultrasound by emergency physicians for the detection of acute limb ischemia, classic positive findings of arterial thrombus can decrease time-to-definitive care.
- Sonographic findings of arterial thrombo-embolic occlusion2:
- Non-compressive artery
- Lack of or altered color doppler flow in artery
- Intraluminal echogenic material in artery
- Optimize your probe position when using color doppler to visualize flow within a vessel (i.e. more parallel to direction of flow), and adjust your scale to suit the flow conditions (i.e. higher flow = higher scale, to optimize your image and reduce aliasing)
- If your images will not be readily available for the surgeon, consider marking the patient to demonstrate the location of the clot