Welcome to another ultrasound-based case, part of the “Ultrasound For The Win!” (#US4TW) Case Series. In this case series, we focus on a real clinical case where point-of-care ultrasound changed the management of a patient’s care or aided in the diagnosis. In this case, a 20-year-old woman presents with first-trimester vaginal bleeding.
Case Presentation
A 20-year-old G1P0 woman presents to the Emergency Department (ED) with several hours of bright red vaginal bleeding. She reports some scant brown discharge earlier in the week, but today developed constant vaginal bleeding. Her last menstrual period was 11 weeks 4 days ago. She states she has had an otherwise unremarkable pregnancy and denies any assisted reproductive technologies (ART) but has yet to have her first obstetrics visit for this current pregnancy. Her review of systems is negative for abdominal or pelvic pain, nausea, vomiting, dysuria, hematuria, passage of clots or tissue, or vaginal discharge or odor.
On physical examination, you examine a well appearing young woman with a soft, non-tender gravid abdomen that appears larger than expected given gestational age. A speculum exam reveals a normal appearing cervix without lesions and blood in the vaginal vault. On bimanual exam, the cervical os is closed with no cervical motion tenderness, and no adnexal masses or tenderness.
Vitals
BP: 143/89 mmHg
P: 90 bpm
RR: 20 respirations/min
O2: 100% room air
T: 36.8° C
Differential Diagnosis
- Ectopic pregnancy
- Molar pregnancy
- Normal pregnancy
- Spontaneous/Missed abortion
- Subchorionic hemorrhage
- Threatened abortion
Point-Of-Care Ultrasound
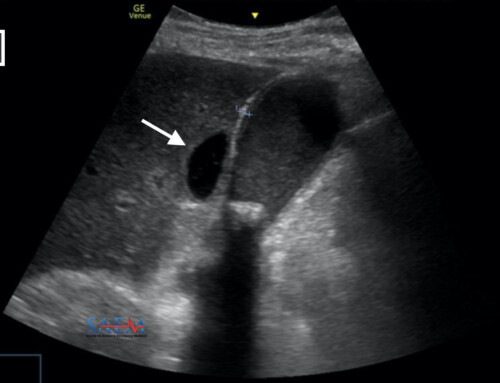
A point-of-care transabdominal ultrasound (TAUS) was performed, demonstrating multiple anechoic areas within the uterus of various sizes in a classic “snowstorm” pattern or “cluster of grapes”, concerning for a molar pregnancy [Figure 1, 2]. A definitive intrauterine pregnancy (IUP) is not identified.

- Figure 1. Transabdominal ultrasound revealing a “snowstorm” or “cluster of grapes” appearance within an enlarged uterus with no definitive intrauterine pregnancy, concerning for complete hydatidiform mole.

- Figure 2. Innumerable anechoic regions of various sizes within the uterus in a complete hydatidiform mole (circled).
Laboratory Investigations
Laboratory studies reveal a mild anemia (hemoglobin 11.1 gm/dL, hematocrit 34.5%) and a markedly elevated quantitative beta-hCG of 943,565 mIU/mL.
Ultrasound Image Quality Assurance (QA)
Emergency physicians play a vital role in the evaluation of patients presenting with first-trimester vaginal bleeding, and point-of-care ultrasound is an invaluable tool that aids in the proper diagnosis. The classic sonographic “snowstorm” appearance of a hydatidiform mole has been used to describe a complex intrauterine mass containing small cystic regions.1
Of note, the term “snowstorm” was described back when image resolution and ultrasound technology was inferior to what it is currently, and a more appropriate description may be a “cluster of grapes”. This finding is more typically seen in a complete hydatidiform mole rather than in a partial mole.1 The sonographic findings of a partial hydatidiform mole may not be as easily identified, and the only evident finding may be an empty gestational sac.1,2 For this reason, ultrasound is only 20% sensitive for identifying partial hydatidiform moles, but highly sensitive (95%) in identifying complete hydatidiform moles.1
The presence or absence of a fetus distinguishes a complete mole from a partial mole. Complete moles are associated with an absence of a fetus, as illustrated in this case, while partial moles are associated with an abnormal fetus or fetal demise.
Finally, if the mass were to be interrogated with color doppler, it would likely reveal high velocity, low resistance flow within the mass.
Disposition and Case Conclusion
Given the point-of-care ultrasound findings suggestive of a complete hydatidiform mole, OB GYN was consulted and a radiology-performed transvaginal ultrasound was obtained, confirming the suspicion of a molar pregnancy. The patient was admitted for a dilation and curettage the following day.
During the patient’s admission, the final pathology returned confirming the diagnosis of a complete hydatidiform mole. Repeat beta-hCG levels however revealed a continued rise after the procedure, and a computed tomography (CT) of the abdomen and pelvis revealed progression of a gestational trophoblastic neoplasia (likely a choriocarcinoma) with an invasive component. Multiple small pulmonary nodules and intra-abdominal lymphadenopathy were evident on CT. The patient was started on systemic chemotherapy with methotrexate by gynecology/oncology.
Discussion
Hydatidiform mole (molar pregnancy) is part of a spectrum of diseases known as gestational trophoblastic disease, which result from aberrant fertilization. While molar pregnancies are the most common gestational trophoblastic disease, others include gestational choriocarcinomas and placental site trophoblastic tumors.3,4 In the United States, the incidence of hydatidiform mole is not uncommon, arising in approximately 1 in 1500 pregnancies. Of these, approximately 20% of patients will develop progression to malignant sequelae requiring chemotherapy. Although most patients will have non-metastatic molar proliferation, gestational choriocarcinomas and metastatic disease can develop with choriocarcinoma in approximately 1 in 20,000-40,000 pregnancies.4
Molar pregnancies are usually diagnosed during the first trimester of pregnancy and typically present initially with abnormal vaginal bleeding.4 Other signs and symptoms of hydatidiform moles may include an enlarged uterus inconsistent with dates, significantly elevated beta-hCG levels, and hyperemesis gravidarum.3 Emergency physicians can identify the classic features of a complete hydatidiform mole on point-of-care ultrasound, allowing for prompt diagnosis and referral for appropriate initial treatment.
Although the gold standard for diagnosis is histopathologic examination of the products of conception, this is clearly of limited use for patients in the acute setting of the Emergency Department. Significantly elevated serum beta-hCG levels combined with the classic sonographic features describe above are highly suggestive of the diagnosis of a hydatidiform mole. These sonographic features should raise the index of suspicion and prompt referral to OBGYN for early treatment.
Take Home Points
- Hydatidiform mole (molar pregnancy) is a common complication of gestation (1:1500 pregnancies) and is part of a wider spectrum of disease known as gestational trophoblastic disease.4
- Patients with molar pregnancy may present with abnormal vaginal bleeding, an enlarged uterus inconsistent with dates, significantly elevated beta-hCG levels, and/or hyperemesis gravidarum.1
- Ultrasound plays a role in identifying complete hydatidiform moles (95% sensitivity), but may not be useful for identifying partial hydatidiform moles (20% sensitivity).1
- The suspicion of a hydatidiform mole requires consultation with OB GYN for appropriate management, including dilation and curettage.