EM ReSCu Peds 5: Diabetic Ketoacidosis
Play this case online for free with Full Code
Brief Narrative Description of Case
The patient’s parents brought her in for vomiting, and “tiredness.” The whole family has had the flu for the past week and all three children were home from school with fever, myalgias, diarrhea. She had a negative COVID-19 swab at a community testing site yesterday. Her siblings seem to be feeling better, but she hasn’t improved yet. She is somnolent, ill-appearing, and severely dehydrated. She is in early hypotensive shock with poor perfusion. Intravenous access attempts will be minimally effective (22g only x 1). She is hyperglycemic, and there is difficulty obtaining additional vascular access. She is hypokalemic (DKA plus diarrhea) and acidotic, which should prompt recognition of DKA with complications.
Management will require IV access (IO), appropriate fluid resuscitation, insulin drip, potassium replacement and admission/transfer.
Primary Learning Objectives
At the end of this simulation, participants should be able to:
- Describe signs/symptoms of shock in a child (comprehension)
- Demonstrate early evaluation of a critically ill patient (application)
- Interpret signs/symptoms of DKA including hyperglycemia and acidosis (evaluation)
- Construct and implement an initial management plan for a child in DKA (application)
- Consider risks of aggressive fluid administration in the setting of DKA such as cerebral edema (evaluation)
- Manage hypokalemia and hyperglycemia in the setting of insulin administration (application)
- Demonstrate focused history taking from a caregiver (application)
- Effectively communicate diagnosis and management to caregivers and respond appropriately to their concerns (synthesis)
- Demonstrate teamwork and closed loop communication (application)
Critical Actions
- Assign/assume team roles
- Obtain brief history from parent
- Place patient on continuous cardiac monitor
- Obtain a point of care glucose
- Establish vascular access – consider IO or ultrasound guided peripheral IV (USGPIV)
- Obtain a venous/capillary blood gas to establish electrolytes/pH level
- Perform focused physical exam/primary survey
- Verbalize diagnosis of DKA
- Initiate appropriate fluid resuscitation for severe DKA
- Initiate appropriate medications (insulin, potassium)
- Communicate effectively with PICU +/- Endocrine consultants
- Explain diagnosis to parent(s) and how it relates to the patient’s presentation
- Effectively manage anxious family members
Case Creators
Authors
- Kimberly Schertzer, MD, FACEP
- Melissa Hersh, MD
Editors
- Ilana Bank, MDCM, FRCPC, FAAP
- Rebekah Burns, MD
- Sherri Rudlinsky, MD
- Josh Davis, MD, NASM-CPT
- Myto Duong, MD
Updated March 29, 2023
Setup
Chief complaint: Vomiting and lethargy
Patient age: 8 years old
Weight: 30 kg
Recommended Supplies
- Manikin: Any model to reflect age of patient (8 years old)
- Moulage: None
- Resources: PALS card and/or length-based tape (e.g., Broselow), local DKA pathways/procedures, if applicable
- Manikin set up: IV line available x 1 in place with drainage bag
- Equipment:
- Point of care tester (for glucose/VBG/K+)
- Intraosseous equipment including E-Z IO, needle, stabilizer, and connectors; saline flushes
- ECG machine
- Cardiac monitor
- Continuous oximeter
- Pediatric airway equipment of various sizes/airway cart
- Simple facemask
- Non-rebreather
- Nasal cannula
- Oxygen tubing
- Suction
- Medications: Normal saline, IV insulin, sodium bicarbonate, mannitol, hypertonic saline, ondansetron (ODT or IV), D10 1⁄2 NS (optional)
Supporting Files
- Point-of-care labs (VBG/CBG, glucose, electrolytes)
- First ECG showing sinus tachycardia with signs of hypokalemia
- Second ECG (if insulin started without checking/giving potassium) showing Torsades de Pointes
Participants/Roles
- Participants/Learners:
- Team Leader
- Airway Manager
- Survey Physician
- Bedside RN
- Medication Preparer
- Medication Giver
- +/- Family Liaison
- Consultant (PICU or Endocrine)
- Embedded participants can play a nurse, respiratory therapist, or tech.
- Standardized patient (actor or faculty) to play patient’s parent
Team roles may need to be adjusted in order to suit local practices and norms
Prerequisite Knowledge
- Faculty
- PALS protocols
- General knowledge of emergency medicine
- Simulation implementation and debriefing experience
- Emergency medicine residents
- Any stage of training (PGY-1,2 for basic case, PGY3+ advanced case)
- Completed PALS certification
Case Alternatives
- If residents fail to recognize DKA within 5 minutes of the case (e.g., gives normal saline boluses, +/- administers antibiotics, +/- gives pressors), the patient will become more lethargic (cerebral edema) and will need emergent airway management.
- If intubation is performed, the patient will become more acidotic and hypotensive.
- For advanced learners, the initial ECG will show u-waves and a wide QRS. If this is not recognized, the patient will develop torsades (and ultimately ventricular tachycardia if not recognized). (See Stage 2)
Virtual Resus Room
This simulation case can be run virtually using Google Slides and Zoom from the Virtual Resus Room (Peds DKA) page.
Milestones
PC1. Emergency Stabilization
PC2. Performance of Focused History & Physical Exam
PC3. Diagnostic Studies
PC4. Differential Diagnoses and Management
PC5. Pharmacotherapy
PC9. General Approach to Procedures
PC14. Vascular Access
PC15. Medical Knowledge
ICS1. Patient Centered Communication
ICS2. Team Management
Resources
- Kuppermann N, Ghetti S, Schunk JE, et al. Clinical Trial of Fluid Infusion Rates for Pediatric Diabetic Ketoacidosis. N Engl J Med. 2018;378:2275-2287. PMID 29897851
- Wolfsdorf J, Glaser N, Sperling MA. Diabetic ketoacidosis in infants, children, and adolescents: A consensus statement from the American Diabetes Association. Diabetes Care. 2006;29:1150-1159. PMID 16644656
- Wolfsdorf J, Craig ME, Daneman D, et al. Diabetic ketoacidosis. Pediatr Diabetes. 2007;8(1):28-43. PMID 17341289
- Glaser NS, Stoner MJ, Garro A, et al.; Pediatric Emergency Care Applied Research Network (PECARN) DKA FLUID Study Group. Serum Sodium Concentration and Mental Status in Children With Diabetic Ketoacidosis. Pediatrics. 2021 Sep;148(3):e2021050243. doi: 10.1542/peds.2021-050243. Epub 2021 Aug 9. PMID: 34373322.
- Kuppermann N. Pediatric DKA: Don’t Fear the Fluids! EMRA Cast, 2020.
- Glaser N, Kuppermann N. A Sweet New Year to All – DKA. PEM Podcast, 2020.
- Woods J, Bukowski J. PEM Pearls: Treatment of Pediatric Diabetic Ketoacidosis and the Two-Bag Method. Acad Life in Emerg Med, 2017. .
| ITEM | FINDING |
|---|---|
| Overall Appearance | An 8-year-old girl is laying on her bed. Her very anxious mother is at her bedside. She is awake and answering questions appropriately but is clearly miserable, clutching her vomit bag and complaining that her stomach hurts. She has tacky mucous membranes. Note: If using a low fidelity mannequin, the team is to refer to the facilitator. If using a high-fidelity mannequin, the team is to refer directly to the mannequin for feedback. |
| HPI | The patient is volunteering very little; she is mostly complaining of generalized abdominal pain (although unable to help pinpoint a specific location for the pain) and anxious about vomiting – although she doesn’t while the medical team is bedside. The mother has limited medical knowledge – and is very anxious that her child will need surgery as she had a friend whose child recently needed stomach surgery. The vomiting and nausea are upsetting her tremendously. Mom will voluntarily share history that the entire family had a cold last week, and everyone improved except the patient who seems worse. Any other history needs to be elicited – and mom will respond to the best of her abilities. She is anxious to help. If the learners ask for specifics:
|
| Past Medical/Surgical History | None |
| Medications | No chronic daily medications – mom has given her daily ibuprofen and cough syrup for her “flu” over the last few days |
| Allergies | None |
| Family History | None – If ever specifically asked, mom comments that maternal grandmother has problems with her sugars |
| Social History | No pets, no smokers, 2 siblings, and 2 parents at home |
Hyperglycemia
Evaluation to identification of DKA
Critical Actions
- Team leader assigns tasks
- Obtains brief history from parent
- Performs primary survey
- Request patient placement on continuous cardiac monitor
- Performs focused physical exam
- Verbalizes recognition of shock
- Obtains point-of-care glucose (high)
- Obtains vascular access
- IO or ultrasound-guided peripheral IV preferred, if peripheral access is unsuccessful
- Verbalizes recognition of hyperglycemia
- Obtains point-of-care VBG/CBG and electrolytes (abnormal)- if extended electrolytes are ordered (Mg+, PO4-, they are not available during case)
- Verbalizes hypokalemia on POC testing OR obtains ECG showing hypokalemia-related changes
- Discusses progress/plan of care with the family
* Unbolded items may be excluded depending on local practices and norms
Physical Exam
| ITEM | FINDING |
|---|---|
| Vital Signs | T: 98.5oF, HR: 130, BP: 90/60, RR: 35, SpO2: 99% on RA, Wt: 30 kg |
| General | Tired appearing, but arousable and alert and oriented x 3. If residents specifically ask, there is a fruity odor to her breath. |
| HEENT | Unremarkable except tacky mucous membranes. Eyes are normal and not sunken. |
| Neck | Unremarkable – no stiffness |
| Lungs | Clear – but if residents ask, there is Kussmaul breathing (deep rapid breathing) – (Some manikins can do this) |
| Cardiovascular | Tachycardia only, no muffled heart sounds |
| Abdomen | Non-distended, patient complains of overall discomfort but no point tenderness |
| Back | No CVA tenderness |
| Neurological | Alert and oriented, but very tired. GCS 14, otherwise normal exam |
| Skin | Dry with cool extremities, capillary refill is delayed 4 seconds, no edema |
Instructor Notes: Changes and Case Branch Points
| INTERVENTION / TIME POINT | CHANGE IN CASE | ADDITIONAL INFORMATION |
|---|---|---|
| Placed on monitors | Vitals are displayed on monitors | Failure to do so within 5 minutes will result in rapid deterioration of patient down cerebral edema pathway. |
| Team attempts/asks for intravenous line x 2 | Initial attempt results in one 22G peripheral IV | If residents fail to get second access, patient’s mental status will start to deteriorate. |
| IV fluid bolus (normal saline 10-20 mL/kg) | Bolus started | Residents will initially order bolus of 20 mL/kg but reduce to 10 mL/kg over first hour after getting blood glucose level. Practice variation exists with management of DKA (fluid quantities and rates, insulin drip dosing). Learners should follow local standards and practices. |
| POC glucose obtained | Result will be 392 mg/dL– should prompt residents to immediately consider DKA. An elevated blood glucose level should prompt discussion to either decrease the IVF rate (to 10 ml/kg) vs keep same (* point for discussion in debrief based on new and old studies- still controversial). | If no POC glucose ordered, RN prompt “Do you want any POC tests?” |
| Asks for IVF to be adjusted to 10 mL/kg following glucose result | Fluid volume will be adjusted. | Nursing staff can prompt with question, “Do you need me to adjust the fluid rate at all?” Mom will ask why fluid rate was adjusted and resident will mention that there is a potential for risk of cerebral edema. Mom will be content with this answer. If learners do not decrease fluid rate, the patient will still be fine, but can bring up as a point of discussion the different management options and the controversial nature of the subject. |
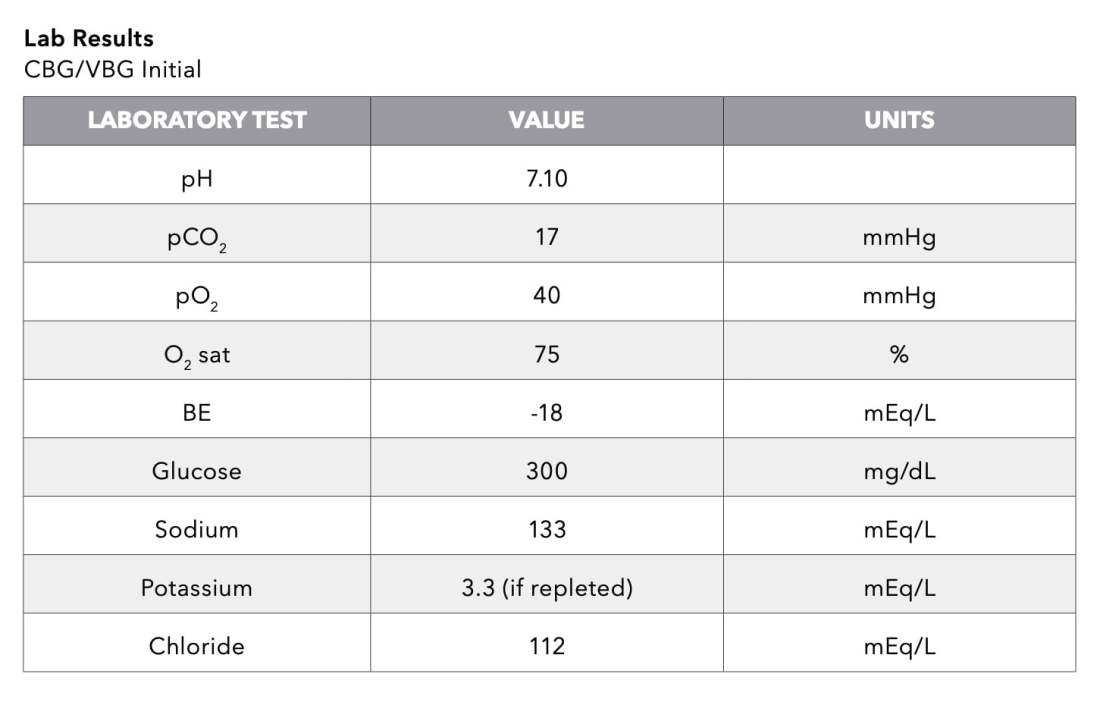
| VBG |
| |
| POC serum electrolytes (K+) | Potassium level is 3.1 mEq/L | If learners don’t order POC potassium, the lab will result during Stage 2. |
| Urine ketones | Learners are told the urine will be collected with the next void. | |
| CBC ordered | Learners are told results will be available in the standard time for site. They may order antibiotics. | |
| Insulin ordered (0.05-0.1 U/ kg/hr) | When insulin is ordered, RN should prompt with, “it will take a couple of minutes to come from pharmacy.” If no POC K+ has been ordered, RN verbalizes need to hold insulin until potassium resulted. Should residents fail to check potassium, can consider ECG changes on monitor (torsades de pointes) and prompt that pathway after insulin started. | |
| ECG ordered after POC labs checked | ECG #1 provided (sinus tachycardia with signs of hypokalemia) | |
| Ondansetron ordered | Medication is given, and this provides patient and mom with a lot of comfort | Consideration of hypokalemia already and potential for prolonged QTc |
| If learners do not verbally identify DKA in first 10 minutes | Increase BP from 90/60 to 150/100 and HR will drop to 80 | Cerebral edema will occur if delay in case progression |
| Patient intubated | If intubated, patient will deteriorate with HR increasing to 150, BP dropping to 70/50, and new VBG/CBG will be 6.9/25/2 | |
| Team member states concern for DKA and summarizes next steps | Proceed to Stage 2. | If this does not occur by 10 minutes, RN asks, “What do we think is happening?” |
DKA Stabilization
Identification of DKA through start of insulin drip and IV fluids
Critical Actions
- Verbalize recognition of DKA, complicated by hypokalemia
- Administer 10 mL/kg normal saline for moderate dehydration
- Reassess perfusion status following initial bolus
- Reassess mental status following initial bolus
- Reassess glucose level following initial bolus
- Begins IV insulin AFTER saline bolus is completed (0.05-0.1 units/kg/hour)
- Begins IV potassium for K<3.5 mEq/L (0.5 mEq/kg over 1 hour) – can be given peripherally as bolus
* Unbolded items may be excluded depending on local practices and norms
Physical Exam
| ITEM | FINDING |
|---|---|
| Vital Signs | T: 98.5oF, HR: 121, BP: 98/70, RR: 28, SpO2: 98% |
| Exam Changes |
|
Instructor Notes: Changes and Case Branch Points
| INTERVENTION / TIME POINT | CHANGE IN CASE | ADDITIONAL INFORMATION |
|---|---|---|
| Potassium bolus ordered (0.5 mEq/kg over 1 hour) | Infusion | Potassium bolus should be ordered either as a bolus or in the 2-bag system IVF. If not given prior to or in conjunction with starting insulin, torsades should develop. |
| Participants formulate a broad differential: 10 minutes after insulin infusion ordered | Insulin arrives from pharmacy and infusion started. Proceed to Stage 3. | If the participants do not come up with at least 5 life threatening etiologies on their differential, the nurse can say “What else could this be?” Attending can intervene and guide with thoughtful and intentional questions if the participants go off track. |
| Initial 10 mL/kg bolus completed | Capillary refill normalizes. No prolonged cap refill. Defer 2nd bolus. Start maintenance IVF + K. | Practice patterns vary here:
|
| Maintenance fluids ordered | RN or tech obtains an ECG. Participants will be shown ECG immediately after completion. | If no comment about additional IVF, RN may prompt with “That first bolus is done, do you want any more?” Example: 1.5 x mIVF + 0.5 mEq/kg mEq KCl See Stage 3 regarding 2-bag system. |
| If no K+ ordered as bolus or in maintenance fluids | K+ levels drop significantly to K 1.5 mEq/L, and torsades will ensue. | Management of torsades with a pulse:
|
| PICU consult and/or Endocrine Consult | The PICU team agrees to open up a bed but asks the ED to manage for the next hour or two. Proceed to Stage 3. |
Case Conclusion and Disposition
Time 1 hour after arrival through reassessment (physical exam and labs)
Critical Actions
- Verbalize need for repeat neuro checks for cerebral edema evaluation
- Verbalize need for q 2 hour electrolyte/glucose monitoring
- Orders VBG + electrolytes STAT if worse in any way
- Explains diagnosis to parent and how it relates to the patient presentation
- Consults PICU and/or Endocrine for admission (if not done in Stage 2)
* Unbolded items may be excluded depending on local practices and norms
Physical Exam
| ITEM | FINDING |
|---|---|
| Vital Signs | T: 98.2oF, HR: 111, BP: 110/88, RR: 22, SpO2: 99% RA |
| Exam Changes | The patient remains alert and oriented. She still has not urinated. Her capillary refill is now <3 sec. |
Instructor Notes: Changes and Case Branch Points
TIME ADVANCE:
Instructors: please state “time has advanced 1 hour since the patient arrived at the ED.”
| INTERVENTION / TIME POINT | CHANGE IN CASE | ADDITIONAL INFORMATION |
|---|---|---|
| Repeat neurological exam | Mental status improving | |
| Repeat blood glucose | POC glucose 300 mg/dL | |
| If a second NS bolus was ordered | RN prompt “Second bolus completed” | |
| Adjust IVF (2-bag method) – Start the 2-bag method based on the POC glucose obtained now at 300 mg/dL | Discuss 2-bag method of management (details of this discussion are outlined in the debriefing points below) Two-bag method for DKA management: Given her body weight of 30 kg –
Because the patient’s blood glucose is 300 mg/dL,
| NOTE: Practice points differ between various centers. You may use your local centre practice and protocols. |
| Repeat VBG/CBG + electrolytes are completed 1 hour post arrival to ED |
| |
| Discussion with mother about DKA, expectations, admission needs, and immediate management plan | Mom will be appropriately anxious and continues to have poor understanding; NOT aggressive or difficult |
Describe signs/symptoms of shock in a child (comprehension)
Shock is the state where blood flow to tissues/organs flow does not adequately meet the demand. Children are more susceptible to cardiovascular compromise from shock because of both physiologic differences (compared with adults) and their limited reserve.
- In general, hypotension is a late finding in pediatric shock. Assessment of perfusion status (e.g., capillary refill) may give an early indication: delayed capillary refill suggests “cold shock” (cardiovascular or hypovolemic source) and very brisk capillary refill suggests “warm shock” (e.g., anaphylactic or distributive etiology)
- Another early sign of shock in children is tachycardia and decreased capillary refill, compared to a low blood pressure.
Demonstrate early evaluation of a critically ill patient (application)
In general, the evaluation of a critically ill child requires quick assessment of the pediatric triangle (appearance, breathing, color) in conjunction with the primary survey with an emphasis on the clinical status
- Appearance: Mental status, level of arousal, and changes in speech/cry
- Work of breathing: Note presence of abnormal breath sounds, retractions, nasal flaring, grunting, apnea
- Circulation to skin: Note presence of pallor, delayed capillary refill, mottling, cyanosis
Primary survey:
- Airway: Does the patient have a patent airway?
- Breathing: Auscultate for bilateral breath sounds
- Circulation: Assess for presence/absence of pulses and degree of peripheral perfusion, cardiac sounds, liver distension
- Disability: Report Glasgow Coma Scale, examine pupils, D * for dextrose
- Exposure: Allow for adequate visualization of the patient
Interpret signs/symptoms and laboratory changes of DKA including hyperglycemia and acidosis (evaluation)
- Hyperglycemia >200 mg/dL
- Acidosis: Venous pH <7.3 or HCO3– <15 mEq/L
- Glucose and Ketones in urine or ketonemia (BOHB >1 mmol/L)
- Mild DKA (pH: 7.2-7.3) (HCO3-: 10-14 mEq/L)
- Moderate DKA (pH: 7.1-7.2) (HCO3: 5-9 mEq/L)
- Severe DKA (pH: <7.1) (HCO3-: <5 mEq/L)
Construct and implement an initial management plan for a child in DKA (application)
- The initial step in DKA treatment is assessment of dehydration status, weight, and mental status.
- The second step in DKA treatment involves blood testing.
- Point of Care (POC) tests:
- Blood glucose level
- Blood beta-hydroxybutyrate (may not be available POC in all locations)
- Urine ketones (may be found on urine dipstick)
- Lab testing:
- Blood glucose level (for more accurate values)
- Serum electrolytes (including bicarbonate – allows for anion gap calculation)
- BUN/creatinine
- Complete blood count
- pH/pCO2
- Calcium, phosphorous, magnesium
- Point of Care (POC) tests:
- The third step includes medications:
- Saline (see detailed discussion below)
- Insulin
- +/- Potassium
- +/- D10
- Avoidance of bicarbonate (lack of benefit and potential for harm)
Consider risks of aggressive fluid administration in the setting of DKA such as cerebral edema (evaluation)
Cerebral injury (or cerebral edema) is rare. Its clinically significant incidence is between 0.3-0.9% of episodes in children with DKA. (Many or most others with DKA will have subclinical cerebral edema without neurological signs). It is more common in children with DKA than adults, and those with the most severe DKA are at highest risk for the cerebral complications. It may be present prior to DKA treatment or during it (between 3-12 hours after treatment begins). The cause is not completely understood. Early work thought it may be the rate of fluid administration but this is being challenged with current lines of research.
– “Clinical Trial of Fluid Infusion Rates for Pediatric Diabetic Ketoacidosis”: June 14, 2018 — N Engl J Med 2018; 378:2275-2287 (DOI: 10.1056/NEJMoa1716816)
- Risk factors for cerebral injury in DKA:
- Severely acidotic on original presentation
- High BUN on presentation (suggests greater hypovolemia)
- Low pCO2
- Insufficient rise of sodium level when DKA treatment starts
- Younger age (<3-5 yrs old) on presentation (because diagnosis is often delayed)
- Identifying cerebral edema (cerebral edema risk tool):
- Positive if any of the following:
- 1 diagnostic criteria
- Abnormal verbal or motor response to pain
- Posturing (decorticate or decerebrate)
- Double vision or cranial nerve palsy (III, IV, VI)
- Abnormal respiratory pattern (Cheyne-Stokes, apnea, grunting, tachypnea)
- 2 major criteria
- Age-inappropriate incontinence
- Abnormal, fluctuating or declining mental status after therapy begins (including agitation)
- Abnormal heart rate sowing (declining by more than 20 beats) that is not explained by sleep or improved intravascular volume status
- 1 major (above) plus 2 minor criteria (minor criteria listed below)
- Vomiting*
- Headache*
- Lethargy or irritability*
- Elevated blood pressure (e.g., diastolic BP >90 mmHg)
- *Especially if begins/resumes after DKA treatment initiated
- 1 major plus 1 minor criteria (if age <5 years old)
- 1 diagnostic criteria
- Positive if any of the following:
- Management of cerebral edema: Treatment should begin as soon as cerebral edema is suspected.
- Treat increased ICP:
- Avoid drugs that increase ICP
- Elevate head of the bed 30 degrees
- Hyperosmolar therapy:
- First line treatment: Mannitol 0.5-1g/kg IV over 10-15 minutes. May repeat in 30 minutes.
- Second line treatment: Hypertonic saline 2.5-5 mL/ kg over 30 minutes
- Neurosurgery consult for possible ICP measuring
- General Principles:
- IV saline to improve intravascular compromise
- 10-20 mL/kg normal saline or lactated ringers
- Ensure adequate airway and assist ventilation as needed
- Supplemental oxygen as needed to maintain a normal O2 level
- Avoid intubation if possible
- If intubation is necessary, hyperventilate to maintain the pCO2 they had before they decompensated. Reduce this over several hours.
- Treat increased ICP:
Manage hypokalemia and hyperglycemia with potential of hypoglycemia in the setting of insulin administration (application)
Patients in severe DKA may also need supplemental IV potassium. Since the goal of insulin administration is closure of the anion gap, supplemental dextrose may be needed when the serum glucose level falls below 250.
When adding dextrose for glucose <250 mg/dL, you may use the “2- bag method”.
- First, calculate the maintenance rate using the standard formula:
- 4 mL/kg/hr for the first 10 kg body weight
- 2 mL/kg/hr for the second 10 kg body weight
- 1 mL/kg/hr for the remaining weight
- In this case (pt weighs 30 kg): 70 mL/hr
- Second, multiply this by 1.5x.
- In this case: 105 mL/hour
- Finally, determine which percentage of which bag to give.
Two-Bag Method of IV Fluids in Hypoglycemia
Supplies
- 1 bag normal saline
- 1 bag D10NS
- 1 bag D12.5 NS
- PRN dextrose
| IF BLOOD GLUCOSE LEVEL | IV FLUID BAG(S) |
|---|---|
| >300 mg/dL | 1 bag
|
| 251-300 mg/dL | 2 bags
|
| 201-250 mg/dL | 2 bags
|
| 151-200 mg/dL | 2 bags
|
| <150 mg/dL | 1 bag
|
| <100 mg/dL | 1 bag
|
| <70 mg/dL | 1 bag
|
Hypokalemia in the setting of DKA
Hypokalemia on presentation signifies a profound total potassium deficit. Caution with IV insulin and bicarbonate therapy is warranted, because it could further drop the potassium levels. Davis et al. 2016 presented a case of profound hypokalemia associated with DKA (Pediatr Diabetes Feb; 17 (1): 61-65). In this case, the patient’s potassium level was 1.3 mEq/L. 0.3 mEq/kg KCI over 1 hour was initiated and insulin held until potassium level was 2.7 mEq/L.They reported that their institution had a policy which prevented them from giving a more aggressive replenishment of 0.5 mEq/kg over an hour potassium via a peripheral line. They opted to avoid risks associated with central line placements. Additionally, 30 mEq/L potassium acetate and 30 mEq/L potassium phosphate were given at 1.5x maintenance.
PFCCS (Pediatric Fundamental Critical Care Support) recommends a conservative IV potassium replacements regimen:
- If K+ 3.0-3.5 mEq/L, administer 0.25 mEq/kg KCL over 1 hour.
- If K+ 2.5-3.0 mEq/L, administer 0.5 mEq/kg over 2 hours.
- If K+ <2.5 mEq/L, administer 0.75 mEq/kg over 3 hours, with checking of the K level half-way through this infusion.
Demonstrate focused history taking from a caregiver (application)
Evaluation of a critically ill child should include obtaining a history from all possible sources including EMS, old records (if time), and especially caregivers. Paying attention to details such as trauma or recent illness may give hints toward identifying the underlying pathophysiology. A history of polyuria, polydipsia, increased hunger and weight loss may suggest undiagnosed diabetes. Children may present with DKA after a mild illness so a review of systems should also include evaluation for infection symptoms.
Effectively communicate diagnosis and management to caregivers and respond appropriately to their concerns (synthesis)
Compassionate, understandable communication with caregivers is critical, as they are strong partners in the treatment of their children. This should not impede lifesaving treatment, but if at all possible, a member of the treatment staff should be assigned to help communicate with parents. Failure to provide a communication liaison may result in anxious parents that may obstruct care. When not actively resuscitating (as in this case), the physician should be able to communicate with patients throughout the child’s care. For complicated concepts, like DKA, it is important to ensure the caregivers understand the explanations being given to them.
Demonstrate teamwork and closed loop communication (application)
Teams may use different frameworks to improve team dynamics and communication. Below are a few definitions that may be helpful to discuss, adapted from the AHRQ TeamSTEPPS Pocket Guide.
- Brief: Short session prior to start of encounter to share the plan, discuss team formation, assign roles and responsibilities, establish expectations and climate, anticipate outcomes and likely contingencies
- Huddle: Ad hoc team discussion to re-establish Situation Awareness; designed to reinforce plans already in place and assess the need to adjust the plan
- Callout: A strategy used to communicate critical information during an emergent event. Helps the team prepare for vital next steps in patient care. (Example: Leader- “Airway status?”; Surveying provider- “Airway clear”; Leader- “Breath sounds?”; Surveying provider- “Breath sounds decreased on right”)
- Check-back: A closed-loop communication strategy that requires a verification of information ensuring that information conveyed by the sender is understood by the receiver as intended. The sender initiates the message; the receiver accepts it and restates the message. In return, the sender verifies that the re-statement of the original message is correct or amends if not. (Example: Leader- “Give diphenhydramine 25 mg IV push”; Med Prep- “Diphenhydramine 25 mg IV push”; Leader- “That’s correct”)
- SBAR: A framework for team members to structure information when communicating to one another.
- S = Situation (What is going on with the patient?)
- B = Background (What is the clinical background or context?)
- A = Assessment (What do I think the problem is?)
- R = Recommendation (What would I do to correct it?)
- Situation monitoring: The process of continually scanning and assessing a situation to gain and maintain an understanding of what is going on around you.
- Situation awareness: The state of “knowing what’s going on around you.”
- Shared mental model: Result of each team member maintaining situation awareness and ensures that all team members are “on the same page.” An organizing knowledge structure of relevant facts and relationships about a task or situation that are commonly held by team members.
- STEP: A tool for monitoring situations during complex situations. A systematic method to review Status of patient, Team members’ performance and status, Environment, and Progress towards goal.
- Cross-monitoring: A harm error reduction strategy that involves 1. Monitoring actions of other team members 2. Providing a safety net within the team. 3. Ensuring that mistakes or oversights are caught quickly and easily. 4. “Watching each other’s back.”
- CUS: Signal phrases that denote “I am Concerned,” “I am Uncomfortable,” and “This is a Safety Issue.” When spoken, all team members should understand clearly not only the issue but also the magnitude of the issue.






Download Case 5 supporting files
Notes:
- ECG 1 interpretation: ECG with signs of hypokalemia. Image from Dr. Ilana Bank.
- ECG 2 interpretation: ECG with torsades de pointes. Image from Dr. Ilana Bank.
For the embedded participants playing the role of the patient and mother
Case Background Information
You are bringing your daughter to the ED for vomiting and “tiredness.”
Over the past week the whole family has had the “flu,” with intermittent fevers, myalgias and fevers. Her 3 siblings, however, are all feeling better – but she doesn’t seem to be back to herself. Additionally, for the last 2 days she has been complaining of stomach aches with “too many to count” episodes of vomiting (NB/NB). You took her to an urgent care earlier in the day and they told you that some children take longer to recover from illnesses than others. You’re not satisfied with that response.
Who are the Learners?
Emergency medicine residents
This case is specifically aimed at first and second year residents who should have experience in gathering information from patients and families, and standard medical treatments and procedures. They may be less familiar with escalating medical therapies when first measures are not successful.
Standardized Patient Information
Mother: Your demeanor is overall anxious and concerned. You are a nervous parent with limited medical acumen. Interrupt the doctors often with questions – but do not be belligerent or aggressive. You are especially concerned about her stomach-ache and really want to know if she will need surgery. If given space, tell the team about your friend’s daughter who has a stomach-ache and then needed surgery, and then ask repeatedly “is this the same thing?” Her nausea is making you very anxious and want it managed quickly. Something is VERY wrong with your child and you know it. You keep giving her Motrin and Robitussin, but it is not making her any better.
Patient: She doesn’t contribute much. She is awake, tired appearing, not moving a lot on the bed, but intermittently rubs her stomach, clutches her vomit bag (if offered one) and talks about feeling like she might throw up. When examined, she cannot specifically tell them where your pain is – “it’s everywhere.” She is alert and oriented if asked. She is also thirsty if asked.
Patient Information
(Please remember not to offer any of this information, but when asked please respond while remaining in character.)
- CHIEF COMPLAINT: “My stomach hurts.”
- AGE: 8 years old
- ADDITIONAL HISTORY: “I had a cold last week, my whole body hurt and since then I feel crummy.”
- PAST MEDICAL HISTORY: None
- SOCIAL HISTORY: None, no recent travel. They have never left California.
- FAMILY HISTORY: Grandma has trouble with sugars – offer only if specifically asked
- PAST SURGICAL HISTORY: None
- MEDICATIONS: None
- ALLERGIES: No known drug allergies
- IMMUNIZATIONS: Up-to-date
- BIRTH HISTORY: Unremarkable. She was born full term, no medical complications (patient is 8 years old, ok if they don’t ask about birth history)
Potential Dialogue
IMPORTANT: Do not offer unsolicited information. Please allow the learners to ask questions. Do not offer information unless they ask you.
Things Mom could say without being asked:
- “All the vomiting has made her lose weight. She keeps eating but is so skinny. I think it’s the vomiting.”
- “Everyone else got better, why isn’t she getting better?”
- “She is such a healthy child, she is never sick and never complains. I know something is wrong.”
Things you might say triggered by events in the scenario:
| EVENT | YOUR POTENTIAL RESPONSE |
|---|---|
| If residents are not picking up on DKA | You could offer that your daughter wet her bed two nights ago. “She never wets her bed.” |
| If the residents continue not picking up on the diagnosis | You can offer the family history of “sugar problems”. |
The learners enter the room to find a patient who is dry, uncomfortable, and tired appearing – she is mildly somnolent but fully arousable. They immediately place the patient on a bedside monitor and recognize that the patient is in early hypovolemic shock. Access needs to be obtained and might be difficult; the residents can place an IO and an IV fluid bolus should be ordered. Initial blood work should also be ordered at this time – including point of care glucose – the result of which should immediately prompt the residents to move down the DKA management pathway.
After completing a physical examination and obtaining an appropriate history, the learners should note that the patient appears to be worsening – her blood pressure has decreased slightly and remains tachycardic. At this point they discuss the risk of cerebral edema with aggressive fluid management. Patient’s perfusion status remains stable and BP is still above 5% for her age range so conservative management should continue. Insulin is ordered and potassium is measured. Potassium returns 3.1 mEq/L, which should prompt the learners to recognize the need to give potassium (either as a bolus or incorporated into maintenance fluid) prior to the initiation of the insulin drip (regardless of whether they additional IVF). Patient remains stable and starts to hemodynamically improve as the second bolus starts.
No signs of cerebral edema are noted on 1 hr neurologic check. She is admitted to ICU, and the endocrine team is consulted, who will follow the patient in the unit. Prior to the end of the case, DKA diagnosis is explained to the patient and her mother, and DKA education is started.
Anticipated Management Mistakes
- Inadequate IV access: Learners may be hesitant to perform IO/ ultrasound-guided peripheral IV (USGPIV) access. Some may be unfamiliar with it or may be concerned that it is painful or frightening for parents to watch. However, with need for IVF, IV insulin, and potassium, access is critical. Furthermore, in critically ill patients, anticipating a need for access is crucial. While IO access and USGPIV are becoming more mainstream, it may be helpful to have a nurse prompt with “we do this all the time”. If learners fail to recognize how ill the child is, a nurse may prompt with “she seems pretty sick, I worry she may get worse quickly.”
- Intubation of a patient in DKA: It would be unlikely in a patient with a fairly normal mental status for intubation to be considered. However, some learners may bring an element of simulation artifact (“it is sim so this is going to go downhill fast”) to the case. In this scenario, intubation leads to worsening acidosis, and PEA requiring CPR and epinephrine. If the conversation heads toward intubation, it may be helpful to discuss the risk/benefit of intubation in an acidotic patient who is relying on respiratory compensation. It is actually quite dangerous to intubate a patient such as this unless the patient is severely obtunded and not maintaining respiratory effort or protecting their airway. It is very hard to be able to compensate as well as the patient can with a ventilator.
- Excessive fluid resuscitation: Some of our learners may provide aggressive fluid resuscitation in an attempt to normalize heart rate and blood pressure. Concerns for cerebral edema increase with aggressive fluid management. This however, is controversial. Please refer to the Kuppermann et al. trial as a point of discussion.
Feedback
Please complete our brief survey describing your experience.






