Imagine a busy evening shift interrupted by the news that the unstable dialysis patient still has no access. Begrudgingly, you drag the ultrasound into the patient’s room. Buried beneath a layer of muscle, a tiny vein lurks below an intimidating artery with a nerve nestled close by. Making matters worse, the patient is becoming increasingly more frustrated. “This always happens. I told them not to remove my last PICC line,” he notes. The use of ultrasound-guided IV improves successful cannulation and decreases complications, but cases like this have caused many emergency providers to resent, even fear, this basic procedure.1–4 Below, we provide additional techniques to increase your success and to avoid the risks associated with central line placement.
Problem: I can’t see any good veins.
Solution: Look distally.
Traditionally, most practitioners scan proximal to the antecubital fossa when attempting ultrasound-guided access. Consider looking distally while utilizing a shorter and smaller gauge needle. This approach allows for vessel preservation by not injuring more proximal veins. Furthermore, smaller gauge needles often provide adequate resuscitation capabilities (i.e. a 20 gauge needle can infuse 3,900 ml per hour).
In most patients, the radial veins are reasonable candidates for IV placement. Often, these are discounted due to their size and proximity to the radial artery. However, the radius stabilizes these vessels, making them less likely to roll or dislodge the catheter during and after placement. The risk of accidental arterial puncture is small with few permanent adverse effects (<1%).5–7
The “intern vein,” a superficial vein running from the dorsal hand along the radial aspect of the forearm, is another target. When possible, place the catheter proximal to the wrist so the hand can still move easily.
Problem: I only see really tiny veins.
Solution: Look for a Y-shaped junction between veins.
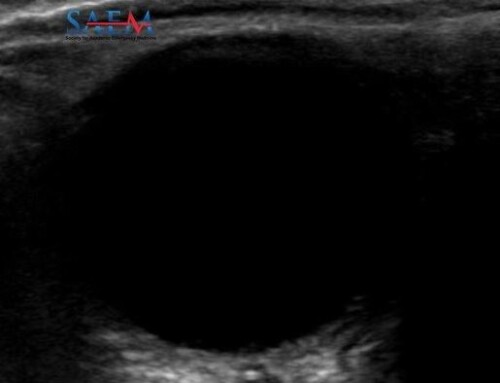
Even small, superficial veins can be cannulated successfully. The typical limiting factor is needle tip visualization and vessel collapse. Minimizing transducer pressure can prevent veins from collapsing, but even then the catheter creates a sonographic shadowing artifact that can confuse the operator regarding the position of the vein and the needle tip.
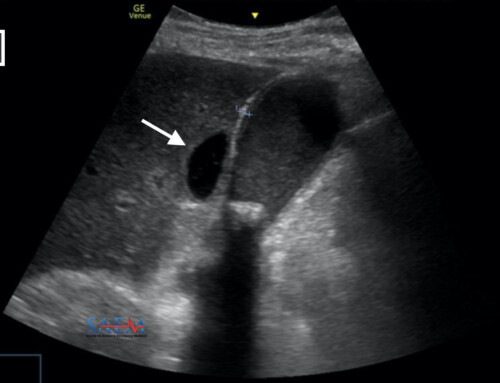
A Y-shaped junction where two veins merge is an especially helpful landmark in situations like this (clip 1). By approaching this venous junction (figure 1), the needle can puncture perpendicularly against the vessel wall while remaining parallel to the overall vessel course.
To cannulate a Y-shaped junction, first mark its location on the skin as well as the direction of each branch distally and proximally. Then, puncture the skin between the distal branches, 1-2 cm distal to the Y-shaped junction. Advance the needle maintaining it between the two distal branches until they converge (clip 2). Continue towards the junction until the needle is visible in the larger more proximal vein.
Problem: I can’t see the needle tip well.
Solution: Move your probe so the transducer is perpendicular to the needle.
Acoustic return is maximized when the needle sits perpendicular to the ultrasound beam, since sound waves can be reflected directly backward to the probe with an angle of incidence of zero. When placing an IV in short axis (transverse view), tilting the probe slightly away from the operator to maintain a 90-degree angle with the needle markedly improves visualization of the needle tip (figure 2). In other words, this tilting (or “heel-in”) maneuver causes the beam to cast somewhat towards the operator and immediately highlights the needle.8 Along the same lines, employing a more shallow angle of insertion can also improve visualization without moving the probe, as can moving the bevel of the needle tip up before or after insertion.

Problem: The vein rolls away from me as soon as I get close to it.
Solution: Try approaching from the side.
Especially in dehydrated patients or those with sclerosed vasculature, veins collapse easily or fade behind artifact as the needle approaches. In these situations, approach the vein from one side rather than from above. To do this, intentionally pierce the skin lateral or medial to the vessel. Advance the needle approximately 1cm until it lies alongside the vein. Then, aim for the vessel from beside it. With this technique, needle artifacts (i.e. reverberation, comet tail, side-lobe, beam-width, or bayonet artifacts) do not obstruct visualization of the vessel.9
Problem: There’s a big brachial vein in the upper extremity, but I can’t get a good angle on it.
Solution: Externally rotate the arm.
In most patients, the brachial vein lies deep to the biceps muscle as it traverses the medial aspect of the upper extremity alongside the brachial artery and median nerve. Its location makes brachial vein cannulation difficult and risky. Nonetheless, it is an invaluable access point for rapid fluid administration and can be a safe option for peripheral vasopressor infusions. To facilitate access externally rotate the shoulder, which often slides the nerve and artery farther away from the vein.
Problem: I get a flash and it seems like the needle is in the vessel, but then I cannot thread the catheter.
Solution: Advance the needle until it is hubbed.
This common scenario is usually because the needle tip is dissecting the inner or outer vessel walls, or because valves and tortuosity impede advancement. In either case, the solution is to advance the needle as far as possible and ensure that the tip is clearly visualized in the vessel (clip 3). Advancing the needle farther causes no additional pain, and navigating it through vasculature is significantly easier, faster, and safer than through soft tissue. Furthermore, directing the needle around curves or into coalescing vessels allows the operator to verify placement more accurately.
Notably, difficulty with catheter advancement is particularly common in the antecubital fossa, where complex venous plexus often forms. While an ideal spot for landmark guided IV access which utilizes a shorter catheter, we recommend avoiding the antecubital veins for sonographic access.
Problem: I still cannot see any veins in the upper extremities.
Solution: Look elsewhere.
Numerous options for ultrasound-guided IV placement exist beyond the upper extremities. These include the external jugular veins and the superficial veins of the lower extremities and abdominal wall. Intraosseous access and central venous cannulation remain viable options as well.
- Looking for pediatric-specific ultrasound-guided IV pearls? Check out PEM Pearls: Pediatric Ultrasound-Guided Peripheral IV Access.
- Worried about your sterile approach? Ultrasound guided peripheral IV: It’s time to clean up our act has you covered.
References
- 1.Costantino T, Parikh A, Satz W, Fojtik J. Ultrasonography-guided peripheral intravenous access versus traditional approaches in patients with difficult intravenous access. Ann Emerg Med. 2005;46(5):456-461. https://www.ncbi.nlm.nih.gov/pubmed/16271677.
- 2.Egan G, Healy D, O’Neill H, Clarke-Moloney M, Grace P, Walsh S. Ultrasound guidance for difficult peripheral venous access: systematic review and meta-analysis. Emerg Med J. 2013;30(7):521-526. https://www.ncbi.nlm.nih.gov/pubmed/22886890.
- 3.Stolz L, Stolz U, Howe C, Farrell I, Adhikari S. Ultrasound-guided peripheral venous access: a meta-analysis and systematic review. J Vasc Access. 2015;16(4):321-326. https://www.ncbi.nlm.nih.gov/pubmed/25656255.
- 4.Vinograd A, Chen A, Woodford A, et al. Ultrasonographic Guidance to Improve First-Attempt Success in Children With Predicted Difficult Intravenous Access in the Emergency Department: A Randomized Controlled Trial. Ann Emerg Med. 2019;74(1):19-27. https://www.ncbi.nlm.nih.gov/pubmed/31126618.
- 5.Brzezinski M, Luisetti T, London M. Radial artery cannulation: a comprehensive review of recent anatomic and physiologic investigations. Anesth Analg. 2009;109(6):1763-1781. https://www.ncbi.nlm.nih.gov/pubmed/19923502.
- 6.Scheer B, Perel A, Pfeiffer U. Clinical review: complications and risk factors of peripheral arterial catheters used for haemodynamic monitoring in anaesthesia and intensive care medicine. Crit Care. 2002;6(3):199-204. https://www.ncbi.nlm.nih.gov/pubmed/12133178.
- 7.Frezza E, Mezghebe H. Indications and complications of arterial catheter use in surgical or medical intensive care units: analysis of 4932 patients. Am Surg. 1998;64(2):127-131. https://www.ncbi.nlm.nih.gov/pubmed/9486883.
- 8.Ihnatsenka B, Boezaart A. Ultrasound: Basic understanding and learning the language. Int J Shoulder Surg. 2010;4(3):55-62. https://www.ncbi.nlm.nih.gov/pubmed/21472065.
- 9.Reusz G, Sarkany P, Gal J, Csomos A. Needle-related ultrasound artifacts and their importance in anaesthetic practice. Br J Anaesth. 2014;112(5):794-802. https://www.ncbi.nlm.nih.gov/pubmed/24566811.