To address the growing issue of physician suicide, the Council of Emergency Medicine Residency Directors (CORD), in collaboration with AAEM, ACEP, ACOEP, EMRA, RSA, RSO and SAEM, annually join forces to help highlight the issues and drive change.
At ALiEM Wellness Think Tank, we tackle resident issues such as preventing suicide and burnout, enhancing resilience, and promoting overall quality of life. Suicide is an important topic that affects our physicians and the future of our specialty. We advocate a culture of support, transparency and openness. If you, or someone you know is exhibiting signs of depression or suicidal ideation, please seek help immediately. Together, we can make the cultural shift to support mental health awareness in medicine and decrease depression and suicide rates.
If you are suicidal and need emergency help, call 911 immediately or National Suicide Prevention Lifeline at 1-800-273-8255 or text 741-741.If you are outside the United States, find a 24/7 hotline at www.iasp.info/resources/Crises_Centres.
Statistics
- About 400 physicians commit suicide every year.1
- According to a Medscape 2019 survey, over 50% of physicians polled had experienced symptoms of burnout and depression, and 14% of physicians had suicidal ideation. In addition, emergency medicine ranks among the top fields of highest burnout rates.2
- High rates of burnout, in addition to other factors, contribute to suicide risk.3
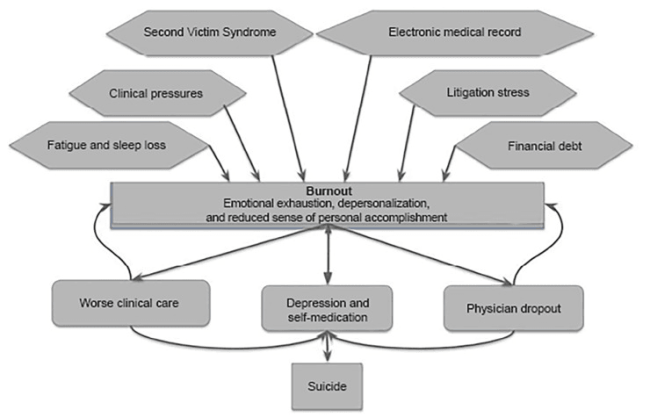
- The suicide rate among male physicians is 40% higher than the general male population.4
- The suicide rate among female physicians is even more pronounced – the relative risk of suicide is 2.27 times greater than the general female population!4
- In a prospective study, 23% of interns had suicidal thoughts. Of those interns, those who completed as little as 4 sessions of Cognitive Behavior Therapy (CBT) reduced the percentage by half.5
- The prevalence of suicidal ideation among medical students is 11.1%, and the prevalence of depression or depressive symptoms is 27.2%.6
- The prevalence of depression among residents is higher than the general population; 28% of residents experience a major depressive episode during training vs. 8% of similarly aged individuals.7
Resources
- Suicide Risk in Physicians Podcast [EMRAP podcast]
- After a Suicide – Toolkit [PDF from American Foundation of Suicide Prevention]:
- AMA Physician Suicide and Support Module
Additional Reading Suggestions
- Physician suicide letters – Pamela Wible
- Why Physicians Die by Suicide [Amazon] – Michael F. Myers
- Interventions to prevent and reduce physician burnout8 – A systematic review and meta-analysis Colin West et al
Identify the warning signs for suicide in yourself or a colleague
- History of major depressive disorder, bipolar disorder, anxiety disorder, or borderline personality disorder
- Prior suicide attempt
- Family history of mental health issues and/or suicidal behavior
- History of physical, psychological, and/or sexual abuse
- History of alcohol abuse
- Major life events that affect a person’s stability and support network – divorce, death in the family, etc
- Relationship problems or domestic violence
- Litigation stressors
- Financial struggles
- Professional and social isolation
Steps to take if you identify an at-risk individual
- Open an honest dialogue and ask questions:
- How are you coping with what’s been happening in your life?
- Do you ever feel like just giving up?
- Are you thinking about hurting yourself or feeling suicidal?
- Have you ever thought about suicide or tried to harm yourself before?
- Do you have a plan?
- Do you have access to weapons or things to harm yourself?
- Keep the person engaged and exhibit empathy through listening.
- Take them to a safe place, away from dangerous weapons.
- Contact local hospital, 911, or National Suicide Prevention Lifeline.
The National Council for Suicide Prevention (NCSP) reminds us to “Take 5 to Save Lives”…
- Learn the signs
- Do your part
- Practice self-care
- Reach out
- Spread the word
Learn more at take5tosavelives.org.
Spread the word!
Share this post with your department or residency today!
https://www.aliem.com/2019/09/national-physician-suicide-awareness-day-2019/
References
- 1.Goldman M, Shah R, Bernstein C. Depression and suicide among physician trainees: recommendations for a national response. JAMA Psychiatry. 2015;72(5):411-412. https://www.ncbi.nlm.nih.gov/pubmed/25738529.
- 2.Kane L. Medscape National Physician Burnout, Depression & Suicide Report 2019. Medscape. https://www.medscape.com/slideshow/2019-lifestyle-burnout-depression-6011056?faf=1#1. Published January 16, 2019. Accessed September 15, 2019.
- 3.Stehman C, Testo Z, Gershaw R, Kellogg A. Burnout, Drop Out, Suicide: Physician Loss in Emergency Medicine, Part I. West J Emerg Med. 2019;20(3):485-494. https://www.ncbi.nlm.nih.gov/pubmed/31123550.
- 4.Schernhammer E, Colditz G. Suicide rates among physicians: a quantitative and gender assessment (meta-analysis). Am J Psychiatry. 2004;161(12):2295-2302. https://www.ncbi.nlm.nih.gov/pubmed/15569903.
- 5.Guille C, Zhao Z, Krystal J, Nichols B, Brady K, Sen S. Web-Based Cognitive Behavioral Therapy Intervention for the Prevention of Suicidal Ideation in Medical Interns: A Randomized Clinical Trial. JAMA Psychiatry. 2015;72(12):1192-1198. https://www.ncbi.nlm.nih.gov/pubmed/26535958.
- 6.Rotenstein L, Ramos M, Torre M, et al. Prevalence of Depression, Depressive Symptoms, and Suicidal Ideation Among Medical Students: A Systematic Review and Meta-Analysis. JAMA. 2016;316(21):2214-2236. https://www.ncbi.nlm.nih.gov/pubmed/27923088.
- 7.Mata D, Ramos M, Bansal N, et al. Prevalence of Depression and Depressive Symptoms Among Resident Physicians: A Systematic Review and Meta-analysis. JAMA. 2015;314(22):2373-2383. https://www.ncbi.nlm.nih.gov/pubmed/26647259.
- 8.West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. The Lancet. November 2016:2272-2281. doi:10.1016/s0140-6736(16)31279-x