While the rate of diabetes climbs, the number of patients who are using insulin pumps grows apace. Pumps appeal to physicians because they mimic normal insulin physiology with a consistent basal rate and appropriate bolus doses for meals. This leads to tighter glucose control and smaller variations. For patients, the pumps can be liberating, requiring far fewer injections than a typical multi-dose regimen. Regardless of why your patient has an insulin pump, it helps to know about how they work… for when they don’t.
While the rate of diabetes climbs, the number of patients who are using insulin pumps grows apace. Pumps appeal to physicians because they mimic normal insulin physiology with a consistent basal rate and appropriate bolus doses for meals. This leads to tighter glucose control and smaller variations. For patients, the pumps can be liberating, requiring far fewer injections than a typical multi-dose regimen. Regardless of why your patient has an insulin pump, it helps to know about how they work… for when they don’t.
Background on insulin pumps
Pumps are not a replacement for a fully-functioning pancreas. In technical terms, insulin pumps are an open system – they deliver a constant rate of insulin, but it is still up to patients to determine where their blood sugar is and where it may trend. Thus, patients with pumps still need to count carbs, and check their glucose frequently (often more frequently than those on multi-dose regimens). [1]
Anatomy of the insulin pump
Generally, insulin pumps consist of a reservoir, a microcontroller with battery, flexible catheter tubing, and a subcutaneous needle. When the first insulin pumps were created in the 1970-80’s, they were quite bulky (think 1980’s cell phone). In contrast, most pumps today are a little smaller than a pager. The controller and reservoir are usually housed together. Patients often will wear the pump on a belt clip or place it in a pocket. A basic interface lets the patient adjust the rate of insulin or select a pre-set. The insulins used are rapid acting, and the reservoir typically holds 200-300 units of insulin. The catheter is similar to most IV tubing (often smaller in diameter), and connects directly to the needle. Patients insert the needle into their abdominal wall, although the upper arm or thigh can be used. The needle infusion set can be attached via any number of adhesives, but tape can do in a pinch. The needle needs to be re-sited every 2-3 days. [2,3]
Complications from insulin pump use
The most common complications of insulin pump therapy involve the skin and soft tissue.
- Local reactions to tape and adhesives are common.
- Local allergic reactions to insulin preparations may occur, particularly in patients who have been recently diagnosed with diabetes and are relatively insulin-naive.
- Lipohypertrophy and lipoatrophy are reactions to insulin itself. Lipohypertrophy is more common, and may reflect local action of insulin, as well as the formation of granulation tissue. [2] Areas of focal lipohypertrophy can be mistaken for an abscess, particularly when associated with scarring. Patients may prefer to place the pump needle in these areas because they can become insensate; however, scarring makes insulin absorption erratic.
- Pump cellulitis is often from Streptococcus and Staphylococcus. This infection is often caused by poor preparation of the pump site before insertion. For reliable patients with mild cellulitis and without systemic symptoms, re-siting the needle after good antiseptic preparation is often enough. [3] More severe cases need systemic antibiotics and MRSA testing – as these patients will continue to have indwelling subcutaneous needles in the future. Similarly, insulin pump-related abscesses should be cultured.
- Weirdly enough, tight glucose control itself has been linked to complications. Initiating insulin therapy in patients who are newly diagnosed with diabetes has been linked to temporary bouts of local edema; while generally harmless, there are occasional case reports of patients presenting with anasarca and even frank fluid overload when placed directly on pump therapy. [4]
Insulin pump problems
Problems with the insulin pump present a much more serious challenge, and can involve any portion of the device. While overt software problems in pumps are extremely rare, it is important to realize that patients may inadvertently select the wrong regimen. Additionally, the batteries can fail, or not be changed in a timely fashion. Tubing can easily kink or crack. Reservoirs can leak or not be replenished on time. Subcutaneous needles can frequently slip out. And while pumps are generally good at alarming if insulin is not being pumped, they may not alarm so long as insulin continues to flow… even if the needle is nowhere near the patient. So be sure to check all sections of the insulin pump.
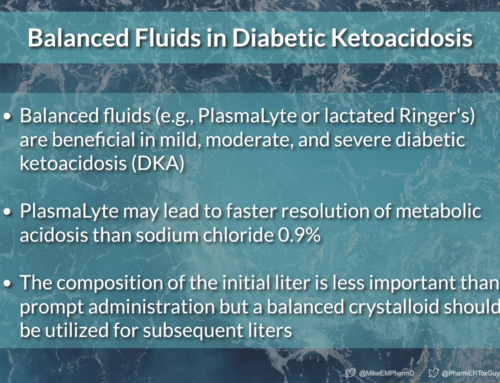
When insulin pumps fail, patients go into hyperglycemic emergencies quickly. The insulins used in pumps are rapid acting and dosed continuously, leaving patients with no depot of insulin if the device fails. Because a malpositioned pump may be noticed several hours late, these patients lack appropriate insulin to compensate for diabetic ketoacidosis (DKA).
Intraperitoneal insulin pumps
Be aware that some patients with particularly brittle diabetes may actually have intraperitoneal pumps. These pumps are inserted into a subcutaneous pocket, like a pacemaker, and deliver extremely concentrated insulin directly into the peritoneal cavity. While implantation makes the pump less likely to kink or become dislodged, these pumps can present with several significant complications common to all implantable devices, such as pocket erosion and hematoma formation, as well as the rare possibility of frank peritonitis. [5]
The coming years are likely to bring major changes in how pumps operate. Closed loop pumps, which include a continuous glucose sensor that is used to drive the basal insulin rate, are likely to become much common. [6,7] While still under development, these systems have the potential benefit of avoiding hypoglycemic overshoots and will help patients to work less to manage their insulin therapy. As pumps continue shrinking, many more patients will present with implantable models. Some groups are beginning to investigate injectable assemblies of nanoparticles that can act as a closed-loop insulin delivery system. [8] So in a few years, your patient’s insulin pump may not even be a pump at all…
Take home points
- Any piece of an insulin pump can fail – the battery, the reservoir, the tubing, or the needle. When troubleshooting, check all the parts.
- A pump often will not indicate that anything is wrong, even if insulin is leaking or the needle isn’t properly positioned.
- Cellulitis at the insertion site is common often caused by poor cleaning or keeping the needle in too long. If it is mild, it will usually get better by just removing the needle.
- Pumps are no match for a Bundt cake. Patients still need to check their glucose levels regularly, because they can become hyperglycemic if they don’t make appropriate adjustments.
- Pumps use short-acting insulin, and patients using them have little to no reservoir. When pumps fail, DKA is just around the corner!
References
- Hoogma, RPLM et al. Comparison of the effects of continuous subcutaneous insulin infusion (CSII) and NPH‐based multiple daily insulin injections (MDI) on glycaemic control and quality of life: results of the 5‐nations trial. Diabetic Medicine. 2006; 23.2: 141-7. Pubmed
- Richardson T, Kerr D. Skin-Related Complications of Insulin Therapy: Epidemiology and Emerging Management Strategies. Am J Clin Dermatol, 2003; 4 (10): 661-667. Pubmed
- Pickup, JC. Insulin-pump therapy for type 1 diabetes mellitus. New England Journal of Medicine, 2012, 366(17), 1616-24. Pubmed
- Rothacker KM, Kaye J. Insulin oedema and treatment-induced neuropathy occurring in a 20-year-old patient with Type 1 diabetes commenced on an insulin pump. Diabet Med. 2013 Jul 1. [Epub ahead of print] Pubmed
- Haveman JW. Surgical aspects and complications of continuous intraperitoneal insulin infusion with an implantable pump. Langenbecks Arch Surg, 2010;395:65–71. Pubmed
- Davis SN et al. STAR 3 Randomized Controlled Trial to Compare Sensor-Augmented Insulin Pump Therapy with Multiple Daily Injections in the Treatment of Type 1 Diabetes: Research Design, Methods, and Baseline Characteristics of Enrolled Subjects. Diabetes Technology & Therapeutics. April 2010, 12(4): 249-255. Pubmed
- Joubert M, Reznik Y. Personal continuous glucose monitoring (CGM) in diabetes management: review of the literature and implementation for practical use.Diabetes Res Clin Pract. 2012 Jun;96(3):294-305. Pubmed
- Gu Z et al. Injectable Nano-Network for Glucose-Mediated Insulin Delivery. ACS Nano 2013 7 (5), 4194-201. Pubmed