Case Writer: Brent Thoma, MD MA
Case Writer: Brent Thoma, MD MA
Case Editors: Teresa Chan, MD and Nikita Joshi, MD
This procedural sedation simulation case can be used to teach, evaluate or reinforce the skills needed to safely perform procedural sedation. It presents a new format for the ALiEM Sim Case Series: Teresa Chan (@TChanMD) has worked magic to amalgamate all of the materials into a cohesive, organized, easy to follow format that also happens to be pretty. The freely downloadable PDF below includes:
- Teacher’s Guide – Provides the information needed for a facilitator to determine if the case is feasible and meets appropriate objectives
- Milestones – Lists the ACGME Milestones that this case addresses
- Case Flow Sheet – Displays a high-level colour-coordinated overview of the case
- Pre-Sedation Patient Information Cards – Displays an outline of the patient’s history and physical exam
- X-ray – Displays the x-ray for the case
- Ketamine Scenario Case Sheet – Lists the changes and complications that will occur if ketamine is used
- Propofol Scenario Case Sheet – Lists the changes and complications that will occur if propofol is used
- Achievement Checklist – Provides a checklist of critical actions that should be taken at each step of the procedural sedation along with pre-written debrief questions to use, if an action is missed.
Download the ALiEM Procedural Sedation Simulation Case
Teachers Guide
Keywords: Procedural Sedation and Analgesia (PSA), Disclosure of Complications
Educational Objectives
Medical
- Understand the characteristics of sedation agents and select appropriate medication
- Perform focused pre-PSA physical exam
- Ensure cardiorespiratory monitoring during and following PSA
- Recognize and treat common PSA complications
Communication
- Acquire informed consent for the PSA
- Respond to nursing challenge regarding the selection of PSA medication
- Communicate effectively as an interdisciplinary team
Case Synopsis
A 62 year old female bent over to tie her shoe and felt her left hip “pop out.” She had a total left hip arthroplasty 4 months ago for progressive arthritis and dislocated it in a similar fashion 2 months ago. It was reduced successfully at that time. She had significant pain initially but now rates it 3/10 and calls it “more of a discomfort.” She has no other complaints and wants the physician to “put the goshdarn thing back” so she can get back to her grandchildren. Her last meal was 6 hours ago and she last drank water 4 hours ago. Your emergency physician colleague has asked for your assistance in sedation so that he can reduce the hip.
Critical Actions
- Complete an appropriate airway assessment.
- Ensure appropriate cardiorespiratory monitoring prior, during, and post procedure.
- Identify and intervene to prevent complications specific for agents administered.
Target Learners
Residents
- Emergency Medicine
- Anesthesia
- Critical care
- Orthopedic
Students
- Medical
- Pharmacy
Location
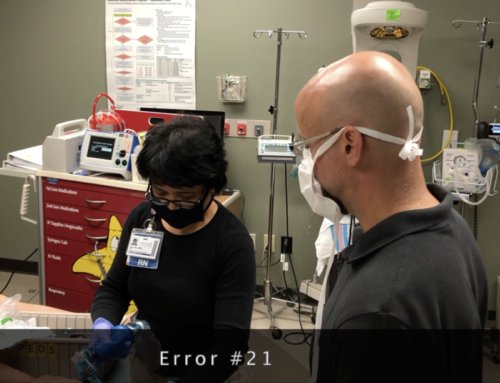
ED resuscitation bay
Patient
62 year old female
Equipment –
- Advanced airway equipment
- Airway adjuncts (if requested)
- Cardiac monitor
- EtCO2 monitor (if requested)
- IV fluid
- Sedation agent
- Syringes
Moulage
Manikin with Street Clothing
Confederates
- Emergency physician colleague – Gives the patient’s history and requests sedation. Attempts to reduce the hip.
- ED nurse – Completes and executes all orders provided. Raises concerns regarding choice of PSA agent with learner.
- Orthopedics attending (voice) – Requests that EP sedate and reduce the hip and call if they have trouble. Agrees to followup as an outpatient.
- Anesthesia attending (voice) – Suggests that patient is appropriate for an ED PSA. Unavailable to assist as there is an urgent case in the OR.
Supporting Files / Media
- Hip x-ray – included in PDF
Translation
BP = blood pressure
ED = emergency department
EP = emergency physician
HR = heart rate
IV = intravenous
LOC = loss of consciousness
PSA = procedural sedation & analgesia
RR = respiratory rate