According to the National Health And Nutrition Examination Survey, approximately 630,000 adults in the United States have cirrhosis of the liver, 69% of which are reportedly unaware of having liver disease. A diagnostic paracentesis is a simple procedure for identifying spontaneous bacterial peritonitis in cirrhotic patients with ascites. A just-in-time training (JITT) model incorporating low-fidelity equipment readily available in the ED can facilitate procedural teaching of the diagnostic paracentesis.
The Innovation: Just-in-Time Procedural Training for Bedside Diagnostic Paracentesis Using the Vacutainer + Needle Technique
This innovation involves just-in-time training (JITT) of the bedside diagnostic paracentesis using a low-fidelity model. Use of this model allows learners to confidently acquire microskills needed to perform bedside diagnostic paracentesis effectively and safely. The technique used in this training minimizes the risk of needlestick exposure to the proceduralist. The materials needed can be easily acquired in most emergency department (ED) and hospital floor settings. The model can be readily used to teach the procedure during an ED shift or scheduled conference time.
The Learners
This innovation targets emergency medicine residents, but can also be applied to other levels of learners, including physician assistants, medical students, and faculty.
The General Group Size
This JITT model may be utilized in a setting with one learner or in a small group of learners.
Case Scenario
A 57 year-old male with a history of alcoholic liver cirrhosis presents with abdominal distention and fever. Upon examining the patient, you note a fluid wave to the patient’s distended abdomen. You have a high suspicion for spontaneous bacterial peritonitis and find it necessary to quickly perform a diagnostic paracentesis.
Equipment Needed for the Procedure
- Bedside ultrasound
- Lidocaine with epinephrine (not required for JITT)
- Chlorhexidine (not required for JITT)
- Vacutainer
- Large bore (18 gauge) needle
- Vacuumed specimen bottles
- Tegaderm or other clear stretchy tape
- 2×2 and 4×4 gauze pads

Supplemental Equipment for the JITT Model
To simulate the abdominal cavity, a 1000 ml bag of normal saline is wrapped in 3 layers of blue disposable underpads (commonly known as “Chux”).
The Technique
- Use point-of-care ultrasonography (POCUS) to:
- Localize a safe pocket of ascites
- Avoid inferior epigastric arteries
- Apply tension in order to perform the Z approach.
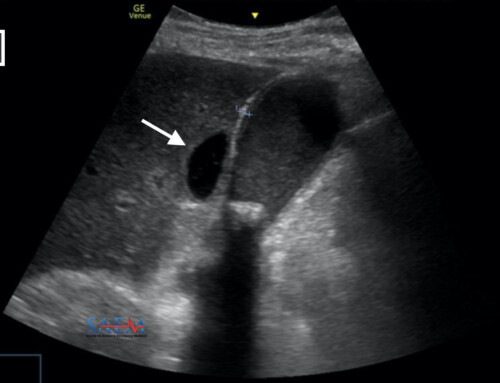
- Push the skin away from or towards the operator to create tension on the surface. This displaces the layers of the skin to allow for the Z approach, which reduces the likelihood of a persistent ascitic fluid leak once the procedure is complete. Notice the proceduralist practicing placement of the pinky finger on the abdominal model, a microskill that allows for stability (Figure 2). For the JITT model, the needle will not be visible on ultrasound because of the absorbent pads used. In the actual procedure, however, dynamic use of POCUS helps localize the fluid pocket and avoid puncture of underlying engorged vessels secondary to portal hypertension.

- Prep the area with Chlorhexidine (not required for JITT).
- Anesthetize using the following options (not required for JITT):
- Lidocaine with epinephrine. Consider shared decision making with the patient, who may elect to skip this step to reduce the overall number of punctures.
- Topical anesthetic. Consider EMLA cream (lidocaine/prilocaine), which requires at least one hour to reach peak effect.
- Topical cooling spray (Gebauer’s Pain-Ease spray)
- Distraction via talking to the patient during the procedure may also help.
- Attach the vacutainer to the needle hub.

- With ultrasound in place to confirm pocket of fluid, insert the needle using the Z-technique.


- Attach vacutainer to vacuum bottles
- As you withdraw the needle, apply firm pressure with gauze.
- Slide the safety protective cover over the needle.
- With the gauze in place, apply the Tegaderm.
- At the completion of the procedure, send the ascitic fluid for the necessary studies to evaluate for spontaneous bacterial peritonitis:
- At least 5 mL should be added to the purple top as it contains anticoagulant and is used for the cell count. Polymorphonuclear (PMN) neutrophis >250 cells/mm3 is diagnostic for SBP.
- Fluid for culture is typically drawn simultaneously, especially if the patient has abdominal pain, fever, acidosis, azotemia, or confusion. Bedside inoculation using blood culture bottles is superior to delayed laboratory culture. Blood culture bottles have also been found to be superior to lysis centrifugation tubes.
- Lactate Dehydrogenase (LDH) less readily enters the peritoneal cavity due to its large size. In SBP, LDH rises such that the ratio of LDH in ascitic fluid/serum approaches 1.0 (normal is 0.4). An LDH ratio greater than 1.0 indicates infection, bowel perforation, or tumor.
- A gram stain is only useful in the setting of perforated bowel as 10,000 bacteria/mL must be present and SBP can be diagnosed with just one bacterial/mL.
- Lactate has not been found to be a helpful measurement in the setting of ascites.

Lessons Learned
Overall, this diagnostic paracentesis JITT model is easy and quick to assemble using materials commonly found in the ED. Use of this model provided an excellent opportunity for teaching of medical student sub-interns. Prior to the beginning of the shift, the model can be assembled within 10 minutes. In between patient encounters, the learners can practice assembling the paracentesis apparatus and performing the technique with the vacutainer.
One learner shared the following perspective:
I really enjoyed the hands on learning. I had never done a paracentesis but had seen quite a few. I felt even more ready to take on the task once I was able to practice the motions using the model. I was the only student on shift and so I got plenty of practice and even felt as though I could teach the next student what I had learned.
Additional lessons learned include that extra absorbent pads are helpful for soaking up the fluid from the punctured saline bag, which will continue to leak. One disadvantage of the model is that ultrasound can not be used to practice visualizing the needle puncture due to the absorbent pad material overlying the saline bag. Despite this limitation, learners can still use the ultrasound probe to practice the microskill of pushing the skin away for the Z approach.
Theory Behind the Innovation
Hands-on learning is rooted in Piaget’s theory of Constructivism, which postulates that learners develop knowledge and meaning based on experience. Procedures are often taught in conference and simulation labs, without the learner actually having to perform the skill on a real patient until a significant amount of time has passed. JITT facilitates teaching of a procedure directly before it is performed on an actual patient in order to refresh a learner’s memory, increase comfort and confidence with the skill, and solidify the information in the learner’s mind by linking it with clinical experience.
Case Conclusion
Your decision to perform a paracentesis confirmed the diagnosis of SBP with a resultant ascites fluid white count of greater than 400 cells. You have already initiated antibiotics and admitted the patient to the medicine service. Blood cultures ultimately return positive for E. Coli, and antibiotics are subsequently tailored according to the resultant susceptibilities.
Helpful References:
Cirrhosis statistics in the first paragraph thanks to: Scaglione S, Kliethermes S, Cao G, Shoham D, Durazo R, Luke A, Volk ML. The Epidemiology of Cirrhosis in the United States: A Population-based Study. J Clin Gastroenterol. 2015 Sep;49(8):690-6. https://www.ncbi.nlm.nih.gov/pubmed/25291348
More innovative educational models from ALiEM’s IDEA series