Case: A 58-year-old male with no past medical history presents to the emergency department for evaluation of right lower quadrant abdominal pain associated with right scrotal swelling. The patient reports that he had a colonoscopy the day before to remove a 20 mm polyp, which had been seen on an outpatient CT scan. He states that he noticed that his right scrotum appeared slightly swollen immediately away after the procedure, but since then the swelling had increased and he developed mild right lower quadrant abdominal pain. Physical examination reveals mild tenderness to the right lower quadrant and swelling of the right scrotum with palpable crepitus of the right scrotum and inguinal canal. There is no overlying skin discoloration. What is the most likely diagnosis?
Pneumoscrotum secondary to iatrogenic colonic perforation
Explanation:
Colonoscopy is a commonly performed procedure which infrequently results in serious complications such as perforation of the colon. Rates of perforation range from 0.03 to 0.8% for diagnostic colonoscopies and 0.15 to 3% for therapeutic colonoscopies.1 Perforation is thought to occur from one of three routes:2
- Direct trauma from the endoscope
- Barotrauma related to over-insufflation
- Trauma from procedures such as clipping or lasering
Physical exam findings to suggest colonic perforation may include:
- Fever
- Abdominal tenderness
- Peritoneal signs (guarding, rigidity, or rebound)
- Crepitus of the abdominal wall or scrotum
Perforation is most commonly diagnosed when free air is seen on radiologic imaging. Iatrogenic colonic perforations may be treated conservatively with bowel rest and antibiotics or surgically. The decision of whether to operate remains controversial and must be made on a case by case basis.3
Once colonic perforation has occurred, gas can travel outside of the peritoneal or retroperitoneal cavity and traverse down into the scrotum, leading to pneumoscrotum. Pneumoscrotum can present immediately after colonoscopy or in a delayed fashion, hours to days later.3 Retroperitoneal perforations are more likely to present in a delayed fashion.3 To date, only a handful of cases of pneumoscrotum after colonoscopy have been described in the medical literature.2 Cases of pneumoscrotum have also been described after pneumothorax, gastric perforation, and traumatic intubation.3,4
Case Conclusion:
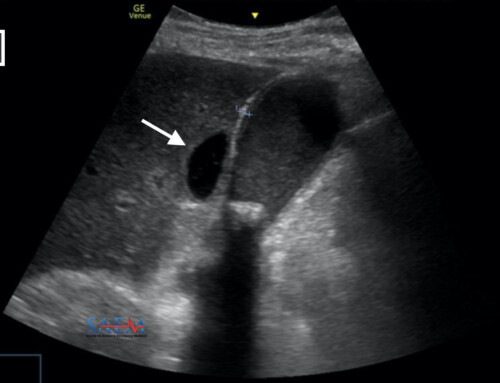
A CT scan was obtained which showed a large amount of intra-abdominal free air, which dissected through the inguinal canal into the scrotal sac resulting in pneumoscrotum. The epicenter of the free air appeared to be near the recently manipulated ascending colon adjacent to where the polyp was resected. The patient was started on IV antibiotics and the general surgeon was consulted, who ultimately decided to take the patient to surgery. During surgery, a large amount of free air was seen but no perforation was found after thorough examination. A drain was placed intraoperatively and the patient was admitted to the hospital. After two days he was tolerating a full liquid diet with no significant abdominal tenderness and had minimal serosanguinous drainage. He was discharged home with the drain and oral antibiotics. A week later, he followed up with his surgeon in the office and the drain was removed. The patient recovered well without any further complications.
Want more visual stimulation? Check out the Diagnose on Sight archives!
References:
- Lüning, T. H., et al. Colonoscopic perforations: a review of 30,366 patients. Surgical endoscopy. 2007;21(6):994-997. PMID: 17453289
- Singh, Sandeep, and Manika Thakur. Pneumoscrotum after colonoscopy. Canadian Journal of Gastroenterology and Hepatology 2008;22(4):411-414. PMID: 18414718
- Fu, Kuang-I., et al. Pneumoscrotum: a rare manifestation of perforation associated with therapeutic colonoscopy. World Journal of Gastroenterology. 2005;11(32):5061-6063. PMID: 2033709
- Millmond, Steven H., and Stanford M. Goldman. Pneumoscrotum after spontaneous pneumothorax with air leak. The Journal of Urology. 1991;145(6):1271-1272. PMID: 2033709