A heavy alcohol drinker, who is well known to your Emergency Department, presents with altered mental status, except that he looks different this time. He looks really bad, stating that he has been vomiting blood. He is hypotensive. He then vomits a copious amount of blood right in front of you. You intubate the patient and initiate the massive transfusion protocol, but everything you pour into him seemingly comes right back out. The gastroenterologist on-call states that he is too unstable for endoscopy. It is time for a balloon tamponade device. You’ve trained for this and set up everything. You call the respiratory therapists (RT) for this mystical “manometer” that you have seen in instructional videos, except that they look puzzled by your request. It is time to MacGyver a method that allows you to know the esophageal balloon pressure that you are generating to avoid an esophageal rupture.

Esophageal Balloon Tamponade Devices – Linton-Nachlas, Sengstaken-Blakemore, Minnesota Tubes (image courtesy of Dr. Mark Ramzy at REBEL EM)
What are esophageal balloon tamponade devices?
There are 2 commonly used devices for tamponading the esophagus during a variceal bleed, the Sengstaken-Blakemore (SB) tube and the Minnesota tube. There is also the Linton-Nachlas tube, but that only has a gastric balloon. The SB tube was created in 1950 in order to help tamponade variceal bleeds [1]. It is a 3-lumen device that has ports to inflate the gastric balloon, aspirate gastric contents, and inflate an esophageal balloon. The Minnesota tube was developed later as a variation to the SB tube and contains an additional port and lumen for aspirating esophageal contents [2]. Another minor difference is that the gastric balloon in the Minnesota tube holds 450-500 ccs of air, while the SB gastric balloon holds 250 ccs of air [2].
Indication: The uncontrolled hemorrhage from esophageal or gastric variceal bleeding after medical or endoscopic treatment fails, is not available, or is not technically possible [3, 4].
Contraindications [4]:
- Unprotected airway
- Esophageal rupture (Boerhaave’s syndrome)
- Esophageal stricture
- Uncertainty of bleeding site
- Well-controlled variceal bleeding
Esophageal balloon tamponade devices achieve hemostasis in 60-90% of cases; however, they are only a temporary measure of hemorrhage control because over 50% of variceal bleeds rebleed after deflation [5].
How do you insert these esophageal tamponade devices?
The following instructions are for inserting a Sengstaken-Blakemore (SB) tube [3, 6]:
- Pre-measure 50 cm above the gastric balloon and esophageal balloon and mark them on the SB tube.
- Fully lubricate the tube.
- Insert the tube similar to an orogastric tube until you have reached the 50 cm mark for the gastric balloon
- Additional trick: You can insert it with a nasogastric tube to have more rigidity and make inserting the tube easier.
- Use a slip syringe at the gastric aspiration site and auscultate to confirm that you are in the stomach. Then fill the gastric balloon with 50 cc of air.
- Verify the placement of the gastric balloon with a chest x-ray.
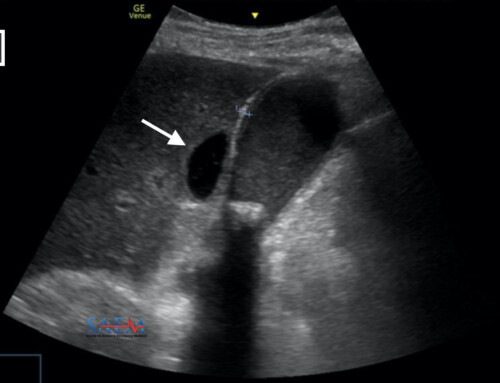
- Additional trick: If the x-ray is delayed, you can pre-check with ultrasound [7]. However final confirmation prior to full inflation should be with a chest X-ray.
- Fully inflate the gastric balloon with 200 more ccs of air for a total of 250 ccs.
- The Minnesota tubes should have the gastric balloon inflated to 450-500 ccs.
- Apply traction to the tube by tying a roller bandage to the end of it and then the other end to a 1 L bag of IV fluids. Then hang the roller bandage over an IV pole.
- Place the nasogastric tube down to the pre-measured level above the gastric balloon and suction the esophageal space. If there is continued bleeding coming from the nasogastric tube then you will need to inflate the esophageal balloon.
- Note that Minnesota tubes already have their own esophageal suction port and will NOT need this NG tube placement to suction the esophagus.
- Use a “manometer” to inflate the esophageal balloon to 30 mmHg. If bleeding persists, you can go to a maximum of 45 mmHg.
What is this “manometer” typically used for the esophageal balloon?
The manometer referenced in numerous videos [6, 8] is actually a cuff manometer, or pressure gauge, to measure endotracheal cuff pressures. Hence, the RT’s are supposed to have them. In our emergency department, the RTs do not spend a lot of time going around measuring cuff pressures and usually save that until the patient reaches the ICU. It is convenient to use for the inflation of the esophageal balloon because it can inflate and measure pressure at the same time.
Pearl 1: Check the units of pressure being used. Manometers often use cmH2O, while esophageal balloons use mmHg.
- The conversion rate is: 1 cmH2O = 0.74 mmHg
- The esophageal balloon goal of 30-45 mmHg is approximately 40-60 cm H2O.
Pearl 2: While the gastric balloon sets a target VOLUME, the esophageal balloon sets a target PRESSURE.
Trick of the Trade: Use a sphygmomanometer as the manometer
Once the inflated gastric balloon is confirmed to be in place, it is time to inflate the esophageal balloon. A manual blood pressure instrument can be repurposed to inflate and measure the esophageal balloon pressure.
- Take your manual blood pressure cuff and detach the connections so you have only a plastic tube that runs to the pressure gauge.
- Connect this plastic tube end to the male Luer lock of a 3-way stopcock.
- Connect the esophageal balloon to a female luer lock on the 3-way stopcock.
- Place a 50 cc syringe on the final female Luer lock of the 3-way stopcock.
- Turn the 3-way stopcock off towards the pressure gauge and inflate the esophageal balloon with 10 ccs of air.
- Then turn the 3-way stopcock off towards the syringe and you should have a reading on the pressure gauge.
- Repeat this using small increments (we chose 10 ccs) until you have a pressure reading of 30 mmHg on the pressure gauge. If bleeding continues, you can increase to 45 mmHg.
Video Demonstration: Esophageal Balloon Inflation
References
- Sengstaken RW, Blakemore AH. Balloon tamponage for the control of hemorrhage from esophageal varices. Ann Surg. 1950 May;131(5):781-9. doi: 10.1097/00000658-195005000-00017. PMID: 15411151; PMCID: PMC1616705.
- Nickson C. Sengstaken–Blakemore and Minnesota Tubes. Life in the Fast Lane • LITFL. Published January 30, 2019.
- Powell M, Journey JD. Sengstaken-Blakemore Tube. [Updated 2022 Jun 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
- Yartsev A. Sengstaken-Blakemore, Minnesotta and Linton-Nachlas tubes. Deranged Physiology. Published July 13, 2015. Accessed April 6, 2023.
- García-Pagán JC, Reverter E, Abraldes JG, Bosch J. Acute variceal bleeding. Semin Respir Crit Care Med. 2012 Feb;33(1):46-54.
- Mason J. Placement of a Blakemore Tube for Bleeding Varices. EM:RAP HD Videos. Accessed December 17, 2021.
- Farkas J. PulmCrit Wee: Ultrasound-guided blakemore tube placement. EMCrit Project. Published May 4, 2016. Accessed April 6, 2023.
- Roohollahi A, Suleiman Bilal Rana H, Hadique S. Blakemore Tube Insertion – BAVLS. American Thoracic Society. Published June 1, 2020. Accessed April 7, 2023.