Diagnosis on Sight: “I have a rapid heart rate”
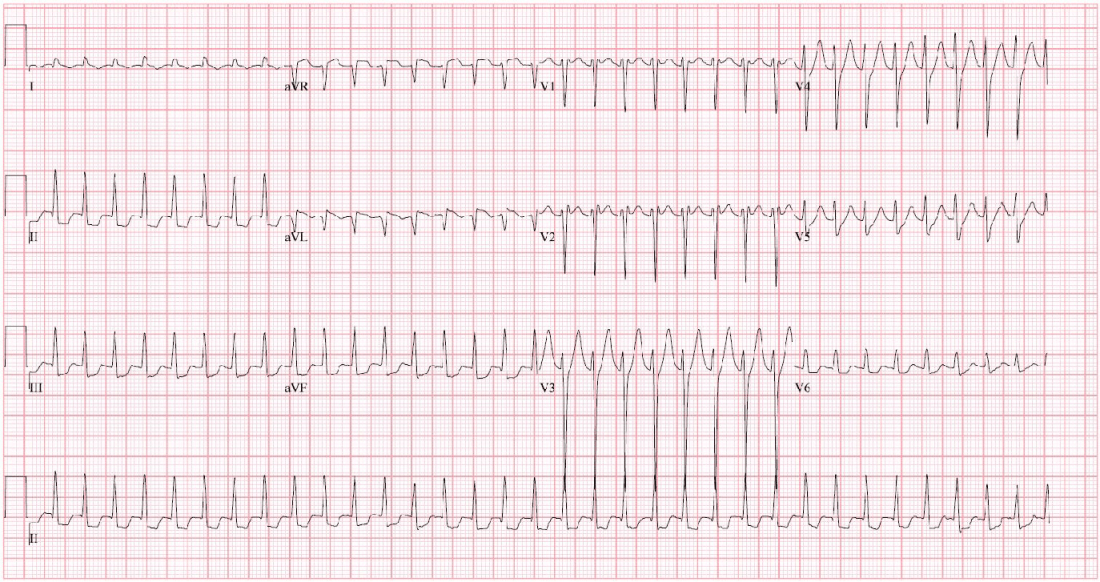
A 31-year-old male presented to the emergency department with palpitations. The patient stated that he thinks his symptoms began “last night” and felt like he had “a rapid heart rate.” He said that prior to last night he felt fine. He did admit to drinking alcohol with his friends 2 nights prior. The patient estimated that he “must have drunk about 30 beers.” On review of systems, he reported feeling anxious. He denied illicit drug use, headache, chest pain, cough, shortness of breath, fevers, nausea, vomiting, abdominal pain, dysuria, or increased urinary frequency. He reported that he was unaware of any family history of early heart disease or sudden death. His initial EKG is shown below.

After consultation with cardiology, the decision was made to cardiovert the patient given the wide complex tachycardia. After cardioversion, the resulting EKG is shown below:
On review of previous records, the patient had a recent ED visit 2 months ago with the EKG shown below:

What is the diagnosis?
Preexcited atrial fibrillation with underlying Wolf-Parkinson-White syndrome
Explanation:
Wolf-Parkinson-White (WPW) syndrome and the WPW pattern on EKG are rare disorders. Only 0.13 – 0.25% of the population have a WPW pattern on EKG [1,2]. However, only a small fraction of these people will develop WPW syndrome. WPW syndrome is defined as a symptomatic arrhythmia with a WPW pattern on EKG.
The patient’s initial EKG showed a wide complex tachycardia that was ultimately determined to be preexcited rapid atrial fibrillation. After cardioversion, the patient’s underlying baseline EKG tracing showed findings of Wolf-Parkinson-White with:
- A shortened PR interval
- Widened QRS complex
- Delta wave: Slurred upstroke of the QRS complex
The most common arrhythmias associated with WPW syndrome are:
- AV Reentrant Tachycardia (AVRT): Seen in over 90% of patients with WPW syndrome [3,4]
- Atrial Fibrillation: 10-30% [5,6]
- Atrial Flutter: Less than 5%
As in this case, AVRT (i.e. SVT) is often followed by atrial fibrillation in patients with WPW. Although the pathophysiology is unclear, up to 35% of instances of atrial fibrillation were preceded by AVRT [5,7,8].
Fortunately, fatal dysrhythmias such as ventricular fibrillation and ventricular tachycardia are very rare with WPW.
Case Conclusion:
Following cardioversion, the patient remained stable in sinus rhythm. After consultation with cardiology, the patient was discharged on Flecainide and Metoprolol and a referral for outpatient cardiology was placed for follow-up care. Soon after, the patient had an electrophysiology study that showed a left posterolateral accessory conduction pathway. He then underwent successful ablation of his orthodromic AVRT.
Want more visual stimulation? Check out the Diagnose on Sight archives!
References:
- Krahn AD, Manfreda J, Tate RB, et al. The natural history of electrocardiographic preexcitation in men. The Manitoba Follow-up Study. Ann Intern Med 1992; 116:456. PMID: 1739235
- Kobza R, Toggweiler S, Dillier R, et al. Prevalence of preexcitation in a young population of male Swiss conscripts. Pacing Clin Electrophysiol 2011; 34:949. PMID: 21453334
- Josephson ME. Preexcitation syndromes. In: Clinical Cardiac Electrophysiology, 4th, Lippincot Williams & Wilkins, Philadelphia 2008. p.339.
- Chugh A, Morady F. Atrioventricular reentry and variants. In: Cardiac electrophysiology from cell to bedside, 5th edition, Zipes DP, Jalife J (Eds), Saunders/Elsevier, Philadelphia 2009. p.605-614.
- Campbell RW, Smith RA, Gallagher JJ, et al. Atrial fibrillation in the preexcitation syndrome. Am J Cardiol 1977; 40:514. PMID: 910715
- Sharma AD, Klein GJ, Guiraudon GM, Milstein S. Atrial fibrillation in patients with Wolff-Parkinson-White syndrome: incidence after surgical ablation of the accessory pathway. Circulation 1985; 72:161. PMID: 4006127
- Sung RJ, Castellanos A, Mallon SM, et al. Mechanisms of spontaneous alternation between reciprocating tachycardia and atrial flutter-fibrillation in the Wolff-Parkinson-White syndrome. Circulation 1977; 56:409. PMID: 884796
- Fujimura O, Klein GJ, Yee R, Sharma AD. Mode of onset of atrial fibrillation in the Wolff-Parkinson-White syndrome: how important is the accessory pathway? J Am Coll Cardiol 1990; 15:1082. PMID: 2312962

 A 76-year-old female with a history of HTN, TIA, CAD, left CEA, and CKD presented to the emergency department for evaluation of neck bruising and swelling. The patient stated that the night before, she was eating popcorn and choked on a kernel. She states that she coughed to clear her throat and shortly after she developed swelling and bruising to the left side of her neck, which has progressively gotten worse. The patient has a remote history of left carotid endarterectomy and was concerned that her symptoms could be related to the prior surgery. On examination, she had ecchymosis and a hematoma/mass to the left side of her neck without palpable thrill or bruit. A well-healed CEA scar was noted. A CTA of the neck was obtained to determine the source of the ecchymosis/hematoma. What is the diagnosis?
A 76-year-old female with a history of HTN, TIA, CAD, left CEA, and CKD presented to the emergency department for evaluation of neck bruising and swelling. The patient stated that the night before, she was eating popcorn and choked on a kernel. She states that she coughed to clear her throat and shortly after she developed swelling and bruising to the left side of her neck, which has progressively gotten worse. The patient has a remote history of left carotid endarterectomy and was concerned that her symptoms could be related to the prior surgery. On examination, she had ecchymosis and a hematoma/mass to the left side of her neck without palpable thrill or bruit. A well-healed CEA scar was noted. A CTA of the neck was obtained to determine the source of the ecchymosis/hematoma. What is the diagnosis?


 Case: A 32-year-old male with a past medical history of diabetes presents with a 1 month history of finger pain after slamming his finger in a car door. 2 weeks after the initial incident he presented to the emergency department for worsening pain and received x-rays that were negative for acute fracture. Today he presents reporting pain radiating up the hand, arm, and into the shoulder, with associated chills. His labs are significant for hyperglycemia, hyponatremia, and an elevated erythrocyte sedimentation rate and c-reactive protein. His x-ray is seen here (figure 1 image courtesy of Daniel Rogan, MD). What is the diagnosis?
Case: A 32-year-old male with a past medical history of diabetes presents with a 1 month history of finger pain after slamming his finger in a car door. 2 weeks after the initial incident he presented to the emergency department for worsening pain and received x-rays that were negative for acute fracture. Today he presents reporting pain radiating up the hand, arm, and into the shoulder, with associated chills. His labs are significant for hyperglycemia, hyponatremia, and an elevated erythrocyte sedimentation rate and c-reactive protein. His x-ray is seen here (figure 1 image courtesy of Daniel Rogan, MD). What is the diagnosis? A 37-year-old female presented to the emergency department for evaluation of numbness and discoloration to her left fourth finger, which had started the day before. The patient stated that she was gardening the previous day and afterward she noticed the discoloration and pain. The patient denied taking any medications. She reported recreational methamphetamine and heroin use. She denied any chest pain or difficulty breathing. She denied any history of Raynaud’s phenomenon, venous thromboembolism, or history of trauma. The patient was afebrile with normal vital signs. Physical exam revealed cyanotic discoloration to the left distal fourth finger. Sensation was intact to light touch and strength was 5 out of 5 in the finger. The capillary refill was diminished. Radial and ulnar pulses were 2+ bilaterally. Initially, a warm pack was placed to the patient’s finger with slight improvement, but without resolution of the pain and cyanosis. What is the diagnosis?
A 37-year-old female presented to the emergency department for evaluation of numbness and discoloration to her left fourth finger, which had started the day before. The patient stated that she was gardening the previous day and afterward she noticed the discoloration and pain. The patient denied taking any medications. She reported recreational methamphetamine and heroin use. She denied any chest pain or difficulty breathing. She denied any history of Raynaud’s phenomenon, venous thromboembolism, or history of trauma. The patient was afebrile with normal vital signs. Physical exam revealed cyanotic discoloration to the left distal fourth finger. Sensation was intact to light touch and strength was 5 out of 5 in the finger. The capillary refill was diminished. Radial and ulnar pulses were 2+ bilaterally. Initially, a warm pack was placed to the patient’s finger with slight improvement, but without resolution of the pain and cyanosis. What is the diagnosis?